Hi, and welcome back to Life as a Cancer Survivor. Jelena here, and today I’m going to talk to you about my experience with telling our daughter Maelle that I have cancer. If you missed my diagnosis video I’ll have the link in the description below to catch you up on any of that. But I hinted in that that we tried to keep her out of the loop at the very beginning because we didn’t know how bad the cancer was so we didn’t want to let her know and have her ask us a million questions that we had no answers for.
 But as a stay-at-home mom with a five-year-old that worked part-time from home, it was going to be really hard to hide all the tests and treatments from her. So we wanted to let her know what was going on early on in the process as soon as we knew what was going to happen. The question would be, how would she handle the news as a five-year-old?
But as a stay-at-home mom with a five-year-old that worked part-time from home, it was going to be really hard to hide all the tests and treatments from her. So we wanted to let her know what was going on early on in the process as soon as we knew what was going to happen. The question would be, how would she handle the news as a five-year-old?
To recap on the timeline of how we got to telling her, May 23rd I had my colonoscopy they found a mass. May 25th we found out that mass was cancerous. May 31st I went in for a CT scan, and a couple days later we found out from that CT scan it hadn’t spread to any organs. But then on June 3rd I had a rectal EUS also known as the rectal ultrasound, and in that it showed that it did spread to lymph nodes so that classified me as Stage 3 Rectal Cancer which meant I was going to be going through radiation and chemotherapy, then I would have surgery, and then possibly eight cycles of chemotherapy after that surgery. So now that we had a clearer picture of what my treatment was going to look like, we felt more comfortable and felt like it was the time to let Maelle know about my diagnosis.
At dinner that evening, after the rectal ultrasound, was when we broke the news to her. I told her that the reason that I had been going to so many doctors’ appointments the past couple weeks was because I have Rectal Cancer. Since she hadn’t been around anyone that had had cancer and didn’t see the bad stuff that it can do to people, she didn’t really get upset or sad by the news. She kind of just saw it as me telling her that I had the flu. I think that was our saving grace at that moment because she didn’t know what to expect so there weren’t any bad thoughts dancing around in her head about what could happen to me.
I explained the basics of all the tests that I had gone through so far, what they had found, that the prognosis was good, and that the cancer was not contagious, but also that I would probably have some rough and tired days ahead as I was going through treatment.
She didn’t have any questions for us after we did all that explaining she just soaked it all in.  I’m sure her little brain was just grinding away trying to figure out and process all that we had just told her.
I’m sure her little brain was just grinding away trying to figure out and process all that we had just told her.
She did get excited when I mentioned that my parents, Grammy and Poppy, were going to be coming for a few weeks to help out while I was going through treatment. So seeing her excitement about that helped relieve some of my nervousness that I had about telling her that I had cancer.
That evening at bedtime she asked me what the tumor looked like. So I said I was able to bring home pictures from my colonoscopy so I can show them to her. She said that she wanted to see them right then, most likely as a bedtime stall tactic, so I told her she’d have to wait until the next morning to look at the pictures.
The next morning I showed her the pictures but she wasn’t really interested in them by then. I could barely even tell what the tumor was in those pictures since I’d never looked at pictures of a colonoscopy before, or a colon in a colonoscopy, so I’m sure she had no idea what she was looking at either. That evening at dinner Maelle asked if the tumor was still in me. So I had to explain to her that yes, the tumor was still in me and it would stay there until I had surgery to actually cut it out of me.
After that one question though she didn’t have any other questions for me. I guess since I didn’t really look or act sick, except in the bathroom, she couldn’t really understand that something really bad was going on inside me. This was her first experience with cancer too, so I think she just had no idea what even to ask.
Although she was only five at the time when I was diagnosed we still wanted to be as open and honest with her through the whole process. A few days later I was sent a link from the radiation oncologist’s office to watch a video on radiation therapy. So I had her watch it with me. I knew some of it was going to be pretty boring, but it showed what the radiation machine would look like so that was good information for her. And it also had a nice video animation of what cells looked like, how normal cells divide and die, and how cancer cells just keep dividing and don’t die.
About halfway through we had to stop the video because she was bored. But she made it through what I thought were the most important parts and the parts that would be the most informative to her.
The next day was my dry run for radiation, so all three of us went down together to the cancer center. I went down to the room where the radiation machine was, did my dry run, and then when I was finished I asked the nurses if John and Maelle could come down and see it, and they said “of course,” so down they came. They were both surprised at the size of the machine, but otherwise Maelle didn’t say much.
We then went to a room to talk to a nurse about the side effects of radiation. Maelle was sitting in my lap playing on her tablet, thought she wasn’t paying attention at all. Then the nurse mentioned that I would probably have diarrhea, maybe even at night time. Maelle perked right up and chimed in, “Mommy might need nighttime undies!”
 I think having my parents come and stay with us for those first three weeks obviously really helped in many ways, but also really helped to serve as a great distraction for Maelle. It gave her two people to play with, which was really important since she was an only child and there weren’t really any young kids in our neighborhood. But it also freed me up to be able to go into my daily treatments without having to drag her with me.
I think having my parents come and stay with us for those first three weeks obviously really helped in many ways, but also really helped to serve as a great distraction for Maelle. It gave her two people to play with, which was really important since she was an only child and there weren’t really any young kids in our neighborhood. But it also freed me up to be able to go into my daily treatments without having to drag her with me.
They allowed her to keep a somewhat normal life by still going to the park for her tennis lessons in the morning, go to the ice rink once a week for a skating lesson, and just go out and have fun and do fun things while I was at home taking a nap. They gave her something going to be excited about rather than just being stuck around me all day and watching me progressively get more and more tired and more sick as I was going through treatment. Obviously I was still getting tired and sick but she had the distraction of Grammy and Poppy there so it wasn’t as in her face.
Telling your child that you have cancer isn’t an easy thing to do, and I’m sure telling an even older child is a completely different beast. Our approach to parenting was to be as truthful as we could with her and talk to her like she was an adult. So naturally, we were going to tell her about my diagnosis and then keep her in the loop as I went through treatment.
If you are a parent that was diagnosed with cancer or have a loved one that was, when did you tell your child or your children about it? Let me know in the comments below.
I hope you’ve been enjoying my videos. Please feel free to share them with anybody that you think might find these useful or helpful. I’d love it if you gave my video a thumbs up so I know that you’ve been liking my videos. And hit that subscribe button. Thank you so much for watching and I’ll see you next week.
*This video was originally published on November 13, 2019
*Link to My Cancer Diagnosis blog post

 The PET scan would show that indeed the lymph node, the enlarged lymph node, in my chest was not cancer but there were multiple lymph nodes involved near the rectum. Ultimately he said that his prognosis for me was that this was curable and that my worst-case scenario would be that I would have a colostomy bag for the rest of my life. Hearing the oncologist say that he believed this was curable was a huge weight lifted off of my shoulders knowing that I was gonna survive this. Curable is not a term that oncologists throw around lightly so I knew that he was confident we were gonna get rid of this nasty cancer.
The PET scan would show that indeed the lymph node, the enlarged lymph node, in my chest was not cancer but there were multiple lymph nodes involved near the rectum. Ultimately he said that his prognosis for me was that this was curable and that my worst-case scenario would be that I would have a colostomy bag for the rest of my life. Hearing the oncologist say that he believed this was curable was a huge weight lifted off of my shoulders knowing that I was gonna survive this. Curable is not a term that oncologists throw around lightly so I knew that he was confident we were gonna get rid of this nasty cancer. therapy and oral chemotherapy. I would go in five days a week for five and a half weeks for pelvic and on those days that I went in for radiation I would also take chemotherapy pills called Xeloda, also known as capecitabine I’m sure I’m pronouncing it wrong but Xeloda is much easier to pronounce and what everyone knows it as. I would take two pills in the morning within about a half-hour of eating and then about twelve hours later I would take three pills in the evening. I was also given a prescription for anti-nausea medication to have on hand in case I got nauseous from the chemotherapy pills. This part of my treatment would start on June 13, 2016.
therapy and oral chemotherapy. I would go in five days a week for five and a half weeks for pelvic and on those days that I went in for radiation I would also take chemotherapy pills called Xeloda, also known as capecitabine I’m sure I’m pronouncing it wrong but Xeloda is much easier to pronounce and what everyone knows it as. I would take two pills in the morning within about a half-hour of eating and then about twelve hours later I would take three pills in the evening. I was also given a prescription for anti-nausea medication to have on hand in case I got nauseous from the chemotherapy pills. This part of my treatment would start on June 13, 2016. Step 2 of my treatment would be major surgery. The doctor that would be doing my surgery preferred to wait 12 weeks after finishing radiation and chemotherapy to do the surgery. He liked to wait that long because after you’re done with those the tumor continues to shrink afterwards. During that surgery, the plan was to remove enough of my colon and rectum that there were clear margins that had no cancer cells in them on either side of the tumor. They would also remove an unknown number of lymph nodes, whatever looked like they were still cancerous that were nearby the rectum. Depending on how much my tumor shrank from step 1 would determine whether or not the tumor was far enough away to save my sphincter muscles and allow me to just have a temporary ileostomy or if they would have to take all of it and I would end up with a permanent colostomy.
Step 2 of my treatment would be major surgery. The doctor that would be doing my surgery preferred to wait 12 weeks after finishing radiation and chemotherapy to do the surgery. He liked to wait that long because after you’re done with those the tumor continues to shrink afterwards. During that surgery, the plan was to remove enough of my colon and rectum that there were clear margins that had no cancer cells in them on either side of the tumor. They would also remove an unknown number of lymph nodes, whatever looked like they were still cancerous that were nearby the rectum. Depending on how much my tumor shrank from step 1 would determine whether or not the tumor was far enough away to save my sphincter muscles and allow me to just have a temporary ileostomy or if they would have to take all of it and I would end up with a permanent colostomy. surgery but was most likely gonna happen just because of my age. Step 3 would take place six to eight weeks after surgery to give my body time to recover from all that slicing and dicing and it would be eight cycles of intravenous chemotherapy called FOLFOX. They wanted to do the second round for what they called mop-up chemo. Since I was so young at diagnosis and the cancer had spread to my lymph nodes they weren’t sure if any stray cells had gotten loose and were swirling around in my lymphatic system just waiting to multiply and spread more. So to make extra sure that they killed all the cancer cells and would give me tons of cancer-free years after this they voted to go aggressive with my treatment and have me do eight cycles of chemotherapy after surgery.
surgery but was most likely gonna happen just because of my age. Step 3 would take place six to eight weeks after surgery to give my body time to recover from all that slicing and dicing and it would be eight cycles of intravenous chemotherapy called FOLFOX. They wanted to do the second round for what they called mop-up chemo. Since I was so young at diagnosis and the cancer had spread to my lymph nodes they weren’t sure if any stray cells had gotten loose and were swirling around in my lymphatic system just waiting to multiply and spread more. So to make extra sure that they killed all the cancer cells and would give me tons of cancer-free years after this they voted to go aggressive with my treatment and have me do eight cycles of chemotherapy after surgery. Step 4 would happen one to two months after my final cycle of chemotherapy if I ended up with a temporary ileostomy. I would have those 1-2 months to recover from those cycles of chemotherapy, build up my strength, build up my immune system, and they would reverse that ileostomy.
Step 4 would happen one to two months after my final cycle of chemotherapy if I ended up with a temporary ileostomy. I would have those 1-2 months to recover from those cycles of chemotherapy, build up my strength, build up my immune system, and they would reverse that ileostomy.
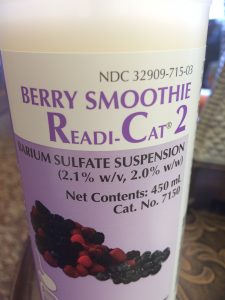 As I mentioned in my last video my colonoscopy doctor got me in touch with the imaging office for me to do a CT scan also known as a cat scan and that was scheduled for May 31st, 2016 at 9:00 a.m. For this CT scan, they had me drink the Barium smoothies, 450-milliliter smoothies, one every hour, and then they had me walk the halls to get it circulating through my body faster. Then at 11 a.m. they called me back, I had to change into scrubs, and then they put the IV into my elbow pit to get me ready for the scan.
As I mentioned in my last video my colonoscopy doctor got me in touch with the imaging office for me to do a CT scan also known as a cat scan and that was scheduled for May 31st, 2016 at 9:00 a.m. For this CT scan, they had me drink the Barium smoothies, 450-milliliter smoothies, one every hour, and then they had me walk the halls to get it circulating through my body faster. Then at 11 a.m. they called me back, I had to change into scrubs, and then they put the IV into my elbow pit to get me ready for the scan.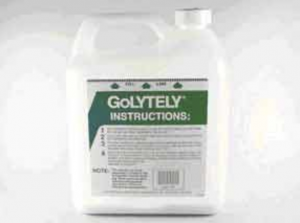 endoscopic ultrasound, also known as a rectal EUS which is what I’m gonna call it for the rest of the video. Since this was another test that uses equipment that goes up your butt to check out things in there it required another colonoscopy prep. This time though I did the ironically named GoLytely prep because you certainly aren’t going lightly after you finish off that gallon jug with the powder.
endoscopic ultrasound, also known as a rectal EUS which is what I’m gonna call it for the rest of the video. Since this was another test that uses equipment that goes up your butt to check out things in there it required another colonoscopy prep. This time though I did the ironically named GoLytely prep because you certainly aren’t going lightly after you finish off that gallon jug with the powder. My final scan was a PET scan, which stands for positron emission tomography, and that was done two days after the MRI. I had to fast for six hours again before this test but this time I didn’t wake up super early in the morning to eat something I slept through the night so dinner was my last meal. When I went back for the scan they told me that the injection was sugar with a radiation tracer and that I would have to lay still in a chair for an hour while I waited for that to circulate through my body so in went yet another IV she tested it with a saline solution to make sure it was working, I got the nasty taste in the back of my throat, so she left to go get the injection.
My final scan was a PET scan, which stands for positron emission tomography, and that was done two days after the MRI. I had to fast for six hours again before this test but this time I didn’t wake up super early in the morning to eat something I slept through the night so dinner was my last meal. When I went back for the scan they told me that the injection was sugar with a radiation tracer and that I would have to lay still in a chair for an hour while I waited for that to circulate through my body so in went yet another IV she tested it with a saline solution to make sure it was working, I got the nasty taste in the back of my throat, so she left to go get the injection.
 So, referencing the last video, May 19, 2016, is the date that I found out I wasn’t allergic to any kinds of foods and gluten-free diet didn’t work, didn’t alleviate the symptoms so I was referred to a colonoscopy. The turnaround was quick so the next day I was at the grocery store buying all the supplies that I needed for my prep…Bisacodyl, Magnesium Citrate, a 14-day supply of powdered laxative (also known as Miralax), and a 64oz. jug of Gatorade…my flavor of choice was lemon-lime.
So, referencing the last video, May 19, 2016, is the date that I found out I wasn’t allergic to any kinds of foods and gluten-free diet didn’t work, didn’t alleviate the symptoms so I was referred to a colonoscopy. The turnaround was quick so the next day I was at the grocery store buying all the supplies that I needed for my prep…Bisacodyl, Magnesium Citrate, a 14-day supply of powdered laxative (also known as Miralax), and a 64oz. jug of Gatorade…my flavor of choice was lemon-lime. even drink water, which sucked because I was thirsty feeling of course once you know you can’t drink any more water, and you can’t even like drink a bunch to trick your stomach into thinking it was kind of full by being full of liquids. No, you’re just stuck being miserable.
even drink water, which sucked because I was thirsty feeling of course once you know you can’t drink any more water, and you can’t even like drink a bunch to trick your stomach into thinking it was kind of full by being full of liquids. No, you’re just stuck being miserable.