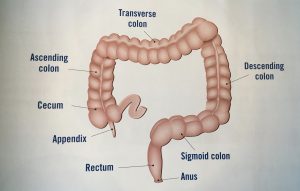
My Story: What It’s Like Having Lower Anterior Resection Surgery
Today’s video is all about my Lower Anterior Resection, also known as LAR surgery which was step two in my treatment plan. It’s one of the most common surgeries that Rectal Cancer patients undergo as part of their treatment myself included. My name is Jelena, and in May of 2016 I was diagnosed with Stage 3 Rectal Cancer. I created this channel to give people like yourself insight on what life is like once you hear those words, “You have cancer.” I also want you to know that you are not alone in your diagnosis and a friend is just a click away. Speaking of click, make sure you’ve clicked on that subscribe button over here so that you never miss any of my new videos. If you’d rather wait till the end of the video, scroll all the way down into the description, and in the description is the link to get you subscribed as well.
Leading up to my surgery I had to stop taking certain medications. Some of the general ones that you have to stop taking include like aspirin and ibuprofen. Then the day before surgery I had two different antibiotics that I had to take to decrease my chances of getting an infection. Then of course since my colon was being operated on I had to do another colon prep, yay. I wasn’t allowed to eat it all that day before surgery and then my colonoscopy prep just was take four stool softener pills and then that 64-ounce jug of Gatorade and the 14 day supply of Miralax mixed together and drink all that up.
of the general ones that you have to stop taking include like aspirin and ibuprofen. Then the day before surgery I had two different antibiotics that I had to take to decrease my chances of getting an infection. Then of course since my colon was being operated on I had to do another colon prep, yay. I wasn’t allowed to eat it all that day before surgery and then my colonoscopy prep just was take four stool softener pills and then that 64-ounce jug of Gatorade and the 14 day supply of Miralax mixed together and drink all that up.
That night I changed the sheets on our bed because according to the surgery instructions you’re supposed to sleep on clean sheets. Then for my shower, I had to use that special soap that they gave me at my pre-surgical appointment and scrub everything for a really long time especially my abdomen and then clean out the belly button very thoroughly. Then once I got out of the shower: no lotion, no deodorant, no perfume, or anything but after taking a shower with that special body wash you’re just so dry and flaky and it’s hard to not put on any lotion. And then I had put on a clean pair of underwear and pajamas.
I was pretty nervous about going in for surgery and waking up with an ileostomy so I didn’t sleep well all that night, but it didn’t really matter too much because since my surgery was first thing in the morning at 7:30 a.m. I had to check-in at 5:30 a.m. And I couldn’t just wake up and go I had to wake up and I had to take that shower again with a special body wash and scrub everything super thoroughly, and then put on another fresh pair of underwear a new pair of clean clothes and then drive the 20 minutes to the hospital.
The one good thing though about getting to the hospital that early is there are plenty of parking spots. My husband and my mom came with me to the hospital and my dad stayed at home with our five-year-old daughter because she didn’t have school that day. Once we checked in at the main desk at the hospital we waited for a few minutes in a waiting area and then were called over to the admission desk. At that admission desk they made sure all of my contact information was right, that they had the right insurance info, that I had my advance directives saved, and then gave me some paperwork to take up to surgery, and gave me my hospital bracelet, and of course verified about 20 million times who I was and what my date of birth was.
I was then sent up to the surgical waiting area which was on another floor in the hospital and gave them my paperwork and checked in at that desk. Ladies, when you check-in, make sure you have to pee because you’re gonna have to take a pregnancy test. We also gave them my husband’s cell phone number in case of an emergency.
 Around 6:30 a.m., about an hour before my surgery was scheduled, I got called back to a pre-op room. They were nice enough to let me bring both my mom and John with me to keep me entertained in that pre-op room. As soon as I got back there they gave me a hospital gown and booties to change into and then they also gave me a hat to put in the pocket of my hospital gown to put on later. Once I was changed then that’s when the warm blankets come out. They’re not very soft, but them being super warm makes up for it.
Around 6:30 a.m., about an hour before my surgery was scheduled, I got called back to a pre-op room. They were nice enough to let me bring both my mom and John with me to keep me entertained in that pre-op room. As soon as I got back there they gave me a hospital gown and booties to change into and then they also gave me a hat to put in the pocket of my hospital gown to put on later. Once I was changed then that’s when the warm blankets come out. They’re not very soft, but them being super warm makes up for it.
Once I was changed, a nurse came in and took my vitals, asked when I had last eaten or drank anything, and made sure that I had completed the colon prep. Then by around 7:00 a.m. a half-hour before surgery, my IV was placed and they hooked me up to just a  hydration drip, which I was super excited about because I was so thirsty having not been able to drink anything since midnight. I also had compression devices put on my calves to help prevent blood clots both during surgery and then for the time after surgery when I still was in bed most of the time.
hydration drip, which I was super excited about because I was so thirsty having not been able to drink anything since midnight. I also had compression devices put on my calves to help prevent blood clots both during surgery and then for the time after surgery when I still was in bed most of the time.
Then the surgeon came in just to say “hi,” see if we had any last-minute questions, then he left to go get ready for my surgery. Then the anesthesiologist came in and had me sign a consent form, and then gave me a little something to help me relax, before he knocked me out. You can tell from this picture how well it relaxed me because I could barely keep my eyes open already from that. I don’t even remember putting that hat on, because after surgery I asked John why they had me put the hat in my pocket if I never wore it.
before he knocked me out. You can tell from this picture how well it relaxed me because I could barely keep my eyes open already from that. I don’t even remember putting that hat on, because after surgery I asked John why they had me put the hat in my pocket if I never wore it.
John and my mom had to head back to the waiting room while I was wheeled off for surgery. Since I was knocked out for surgery I’ve invited my husband John to come in and talk to us about what actually happened while I was asleep so here he is.
John: Hey everyone.
Jelena: Welcome!
John: Thank you.
Jelena: So, what happened when I was taken away for surgery?
John: Yeah, after you’re taken away for surgery there was no expectation that us waiting for you stay at the hospital because it is such a long surgery. They had my cell phone number in case you needed to get a hold with us for any kind of emergency reasons but we started off, your mom and I, went out to breakfast which managed to successfully kill about an hour. After that, we ended up coming back to the hospital and waiting in the surgery area so if that’s what you’re gonna do I would recommend coming with enough stuff to keep yourself busy for about four hours at least four hours. In our case, I think your mom brought some books to read, I had you know games to play on my phone, and I think even at one point I just kind of laid down on one of the couches in the waiting area and decided to take a nap since we had been up since 4:15 in the morning.
Jelena: Okay I guess that’s understandable. So then did you get any updates while I was in surgery?
John: Yeah, we had one update in the middle of the process and the way that it works in our hospital is one of the nurses from the surgery room would call down to the reception desk in the surgery waiting area, and then the receptionist at the surgery waiting area would call you over to come talk to the nurse directly. And in this case you know the update that they gave us that was that everything was going well, everything was going smoothly and according to plan however, it was going to be probably an hour to an hour and a half longer than they had originally estimated because they needed to take some time to free up some extra colon from your abdominal wall in order to actually make the resection.
Jelena: Okay. So then after the surgery was over and you got an update from the surgeon were you able to see me right away?
John: We weren’t able to see you right away. So he came down and he talked to your mom and I in the waiting room and he gave us the update that everything had gone according to plan. There were no complications so there was nothing special that we needed to do outside of what we had discussed before going into surgery. However, we weren’t able to see you right away because at the time you were in the post-anesthesia care unit and they were bringing you back out from being under the anesthesia and eventually you know we stayed in the surgery waiting area for a little while and then eventually a nurse from the post-anesthesia care unit called down to the surgery waiting desk and I spoke to her on the phone. And at that point she gave us the update that you were still in the process of kind of waking up after being under, you were probably gonna be there for another thirty minutes to an hour and at that time she actually gave us the room number that you were gonna be staying in for the recovery portion of your stay at the hospital. So after that phone call, your mom and I left the surgery waiting area, and then we went up to the room that you would actually be staying in.
Jelena: Oh okay, nice. So was that a little more comfortable than the waiting area?
John: Um, I don’t know if it was necessarily more comfortable it’s still hospital furniture, but it was at least a little more private.
Jelena: Okay. So then what happened once you got to the room?
John: Once we got to the room we were just sitting in there by ourselves. Occasionally one of the nurses would come in and out and they would kind of introduce themselves. So you were staying on a floor that specializes in post-surgical care, so the nurses that were working with you for that piece like that was kind of what they specialized in was people who had just come out of surgery. So as they came in and they talked to us before you were actually in the room they would kind of introduce themselves and say who they were like if they were your main nurse for the time or the CNA (Certified Nursing Assistant). I think at one point the social worker who was in charge of like the in-hospital ostomy nurse visits and who would also be coordinating the um, the homecare afterwards came in and introduced herself to me and your mom. And eventually, they came up with you. So they wheeled you in in the hospital bed into the room at this point we hadn’t we consciously made the decision not to bring any of your stuff up yet because we didn’t know how easy it was to get somebody in and out of the hospital room, and we just didn’t want it to be in the way. So once they brought you in I mean you were really out of it still. It was, you looked like you were just kind of going in and out of sleep, and you kind of were that way for the next two hours. So during that period of time, the nurses actually started the you know the regimens of care that they were gonna do for you after surgery and you know we continued to sort of you know they would come in and they would tell us what they were doing so we got an idea of what they were doing for you and what the plan was, but also during that time since you were fading in and out of consciousness and kind of going in and out of sleep that’s when we decided that we would go down to the car and bring up all the bags that you had packed for your stay.
Jelena: Okay. Well, thanks for filling me out on what happened while I was unconscious.
John: Yeah, anytime.
Jelena: I’m sure I’ll have you back for a future video.
John: Sounds great.
Jelena: Alright, thanks. Bye-bye.
Once I was up there at some point I opened my eyes and saw that I was in a different room, my mom and John were in there so I wanted to try and stay awake but I was still just too groggy and I could not keep my eyes open. I was a little nauseous, so they did give me a cold towel to wear on my head. I looked basically like death as you can see from this picture, which was pretty shocking to my mom.
my mom and John were in there so I wanted to try and stay awake but I was still just too groggy and I could not keep my eyes open. I was a little nauseous, so they did give me a cold towel to wear on my head. I looked basically like death as you can see from this picture, which was pretty shocking to my mom.
Once I was awake enough to talk I asked if my dad could bring Maelle to  the hospital to see me. I really wanted to see her, give her a hug, and show her that mommy made it through surgery okay. Once she showed up though, I still could barely stay awake and I couldn’t even open my eyes and smile to take a picture with her at 4:30 that afternoon.
the hospital to see me. I really wanted to see her, give her a hug, and show her that mommy made it through surgery okay. Once she showed up though, I still could barely stay awake and I couldn’t even open my eyes and smile to take a picture with her at 4:30 that afternoon.
Eventually, around 7:30 p.m. which was 12 hours after my surgery started, I was finally awake enough that I wanted to survey the damage that was done and see everything that was hooked up to me. John had to help me with pulling my blanket up so that I could lift my hospital gown up and not flash everybody when I was looking at my abdomen. I was so sore though that the only way that I could sit up was by using the remote on the hospital bed to raise me up as high as it would go.
Here’s the first picture of my tummy after surgery and don’t worry it’s all bandaged up all you can see is just a little bit of my stoma peeking through the ostomy bag. Up at the top there, the little square with a green probe on it is one of the many stickies I had on me to monitor my heart rate. I of course was still hooked up to an IV, I was hooked up to oxygen, a catheter was put in me during surgery and that was still connected to me, I still had those sleeves on my calves compressing squeezing and letting go of them so I didn’t get any blood clots, and I had a little oxygen monitor on my finger.
bandaged up all you can see is just a little bit of my stoma peeking through the ostomy bag. Up at the top there, the little square with a green probe on it is one of the many stickies I had on me to monitor my heart rate. I of course was still hooked up to an IV, I was hooked up to oxygen, a catheter was put in me during surgery and that was still connected to me, I still had those sleeves on my calves compressing squeezing and letting go of them so I didn’t get any blood clots, and I had a little oxygen monitor on my finger.
Attached to the IV were liquids to keep me hydrated because I was NPO which means “nothing by the mouth”. I know the NPO doesn’t match up with “nothing by the mouth” but it’s something Latin. I was allowed to have ice chips so sucking on that really helped to soothe my throat because it was really dry for some reason after surgery. Also hooked up to my IV was a patient-controlled analgesia pump also known as PCA. Mine had morphine in it and I was given a button that I could push whenever I wanted a dose administered. That button was hooked up to a timer so I could only get a dose every 15 minutes so after I pressed the button the timer would start and when the 15 minutes was up a light would turn on letting me know that I could hit the button again. If you hit the button when the light was off it just wouldn’t do anything. For the first day or so I was hitting that button every time that the light was going on.
 Then a little before 8 p.m. a nurse came in to take the gauze off of my incision. Now is when you may want to look away because it’ll get a little gross and I’ll tell you when it’s okay to look again. So there was a lot of blood on the dressing but the wound itself wasn’t bleeding anymore so she didn’t put a new dressing on it. Okay, it’s safe to look again. After removing the dressing the nurse wanted me to sit up in the chair in the room. The only way that I could get up was by putting the bed as upright as I could at the head, rolling from my back over to my side which was really painful, and then using my arm to push my torso away from the back at the bed so I was sitting up and somehow turning my body so my legs were hanging off the bed actually. I think the nurses had to grab my legs and rotate me because I couldn’t do it. After all of that, I could manage only about 30 seconds sitting upright because I was so out of breath and it hurt so much I had to lay back down. So then they had to help me get my legs back up ’cause I couldn’t even lift my legs up and then I laid back down and put that bed back.
Then a little before 8 p.m. a nurse came in to take the gauze off of my incision. Now is when you may want to look away because it’ll get a little gross and I’ll tell you when it’s okay to look again. So there was a lot of blood on the dressing but the wound itself wasn’t bleeding anymore so she didn’t put a new dressing on it. Okay, it’s safe to look again. After removing the dressing the nurse wanted me to sit up in the chair in the room. The only way that I could get up was by putting the bed as upright as I could at the head, rolling from my back over to my side which was really painful, and then using my arm to push my torso away from the back at the bed so I was sitting up and somehow turning my body so my legs were hanging off the bed actually. I think the nurses had to grab my legs and rotate me because I couldn’t do it. After all of that, I could manage only about 30 seconds sitting upright because I was so out of breath and it hurt so much I had to lay back down. So then they had to help me get my legs back up ’cause I couldn’t even lift my legs up and then I laid back down and put that bed back.
That was so mentally crushing because leading up to my surgery I had been running like three to four times a week three or four miles at a time so to go from that to not even being able to sit up for 30 seconds without feeling like I was gonna die basically, it was hard. The nurses wanted me to try and get up and walk that evening, but after getting so exhausted after just trying to sit up for 30 seconds the thought of me even trying to walk from my hospital bed to the door of my room seemed impossible.
That day of surgery was a huge struggle both physically and mentally. I felt like I had been run over by a dump truck, I couldn’t do anything for myself. I ambitiously thought before I went in for surgery I’d be in and out of the hospital in like three days. That evening after surgery I totally understood why they said my hospital stay was gonna be more like four to seven days. Recovery was gonna be rough but I had no choice but to tackle it head-on.
I’m gonna be taking a break for a couple of weeks because the pressure of keeping up this channel, work, a big sewing project, and just everything at home is starting to stress me out a little bit and I’m feeling my anxiety start to kind of creep back in. But don’t worry, I won’t be gone for long. Hopefully, by mid-March, I’ll be back and better than ever.
Until then you can keep up with me on Instagram my handle there is colorado.jelena or on Twitter my name is Survivor_Jelena. I’ll have the links in the description too so you can just go down there and click on those to follow me. Make sure you share this video with anybody that you think might like it and please hit the like button for me so that YouTube knows that you’ve liked this video and then they’ll share with more people. Thanks for watching and I’ll see you again soon.
*This video was originally published on February 19, 2020














 mark a location on my abdomen where they wanted the small intestine to be sticking out. First, she wanted to know where I usually wore my pants so that she could mark my waistband and make sure that the stoma didn’t fall right on that waistband. Then she marked around my belly button, which had been stretched out from pregnancy. And then she went to the right of the belly button and she made that big mark thereof where the stoma was gonna be going.
mark a location on my abdomen where they wanted the small intestine to be sticking out. First, she wanted to know where I usually wore my pants so that she could mark my waistband and make sure that the stoma didn’t fall right on that waistband. Then she marked around my belly button, which had been stretched out from pregnancy. And then she went to the right of the belly button and she made that big mark thereof where the stoma was gonna be going.




 like the sizes of hairs so my dad tried his best to fix them and splice them back together but normal household tools are just too big to try and get these fixed so I didn’t have them for that hospital stay but any kind of nice noise-canceling headphones would be great.
like the sizes of hairs so my dad tried his best to fix them and splice them back together but normal household tools are just too big to try and get these fixed so I didn’t have them for that hospital stay but any kind of nice noise-canceling headphones would be great.