My Ileostomy Reversal Experience
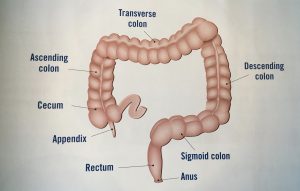
Today I’m going to cover my most requested topic: my ileostomy reversal surgery. So be prepared there’s going to be a lot of poop talk. My name is Jelena and at age 34 I was diagnosed with stage 3 rectal cancer. I had an ileostomy for over 7 months after my lower anterior resection, or LAR, surgery. The LAR surgery it’s where part of your colon and rectum are removed and the new ends they’re sewn together and you get a temporary ileostomy while that resected site heals. An ileostomy is where the end of your small intestine is run out of your abdominal wall to create a stoma and your waste exits your body through there. My ileostomy was reversed on June 4th, 2017 and this is my story on how that went how recovery was and a little bit about how things are today. I’ll also give you some tips on how to survive those first few days post-reversal.
The first step in getting ready for surgery is going in for a Flex Sig, which is short for a flexible sigmoidoscopy. They do this procedure to check and see visually how that resected site where your colon and rectum were sewn together to see how that’s healed. It’s different from a colonoscopy in that the camera – it only goes part of the way up your colon so it just goes up to the site where the colon and rectum were sewn together it doesn’t go through your entire large intestine. My procedure was done at the hospital by my surgeon and the prep for it was easy. All I had to do: I wasn’t allowed to eat after midnight, no drinking after 3:45 a.m., check-in was at 7:30 a.m., and the procedure was at 9:00 a.m. I was knocked out for it and when I woke up I was told that everything looked good and this test was passed. So this test, this procedure, was done five weeks before my ileostomy reversal surgery was scheduled.
Next up was a gastrografin enema test. Gastrografin is a water-soluble clear liquid that shows up on x-ray pictures and this test is done to make sure that there are no leaks at that resected site where your colon and rectum are sewn together. There was no prep for this procedure because they’re only looking in your large intestine and since I had the ileostomy there was no stool in my large intestine and you’re awake for this procedure. First I had to remove all my clothing from the waist down and put on a hospital gown, and while I did that, the tech prepared the gastrografin solution. You lie on your side on a table for this procedure and the first thing that the tech did was insert what was basically a deflated balloon with a tube running through it up my butt just past my sphincter muscles and then inflated that balloon so that the tube wouldn’t come out during the procedure. So that was not very comfortable. Then came the gastrografin so there’s over one liter of this fluid that gets pumped into you slowly into your large intestine. As it’s getting pumped in it gets more and more uncomfortable the more liquid’s in there and I kind of started cramping a little bit because of all that liquid being pumped in. Once the over one liter of fluid is in then you have to hold it inside of you and then the tech proceeds to take a bunch of x-ray pictures of you laying on your side, turning to the other side, on your back, with like your butt up in the air on your back in like a bridge position. It was, um, not comfortable.
When she had finished there was a bathroom connected right to that room and I pretty much just had to walk like six feet to get into that bathroom. So she said that the liquid shouldn’t come out before I get to the bathroom. Well . . . she lied. As soon as I stood up and took my first two steps I could feel some of that liquid dripping down my leg. I mean, my sphincter muscles haven’t been used in months, and even if they had been it’s really hard to hold liquid in, so I just rushed as quickly as I could to the toilet, sat down and a bunch of that fluid came out. I stayed on the toilet for about 10 minutes because I still felt like there was more in there that needed to come out, so there was another like round of the liquid coming out. But then nothing else was coming out, so I assumed all was okay so I got dressed and went home. But once I got home there was one more round of the liquid gushing out of me and then I was okay for the rest of the day. Thank goodness I passed the test and there were no leaks, so that meant I had the full go-ahead to get my reversal surgery.
This time I did a little bit of research ahead of time before going in for my surgery to learn a little bit more about what I should expect and what I should bring to the hospital with me. I only brought one pair of clothes because I knew from my previous hospital visits I wasn’t changing out that hospital gown until it was time for me to go home. I did bring a few pairs of underwear with me, though. I bought some adult diapers to bring with me and some diaper rash cream. I also learned that the usual criteria for letting a person go home after their reversal surgery is they first have to pass gas and then they have to pass a bowel movement. So since I knew I wanted to spend as little time as possible in the hospital, my goal was to take as few pain medications as possible, because those pain medications, they constipate you. So if I was constipated that means that would delay when my first bowel movement would happen.
of underwear with me, though. I bought some adult diapers to bring with me and some diaper rash cream. I also learned that the usual criteria for letting a person go home after their reversal surgery is they first have to pass gas and then they have to pass a bowel movement. So since I knew I wanted to spend as little time as possible in the hospital, my goal was to take as few pain medications as possible, because those pain medications, they constipate you. So if I was constipated that means that would delay when my first bowel movement would happen.
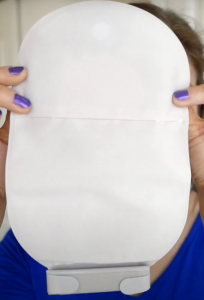
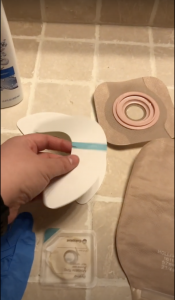
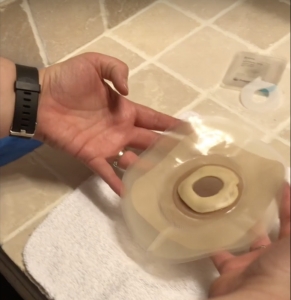
My surgery was scheduled for 9 am on June 5th, 2017. My surgeon was also going to be taking my port out at the same time during the surgery because I was done with treatment and I was declared that I had no evidence of the disease so my oncologist said to go on ahead and get my port removed as well. The mood was definitely a lot different for this surgery versus my LAR surgery. I was excited to go in for this surgery because I couldn’t wait to get that ileostomy reversed. The couple of weeks leading up to this surgery, the skin
taking my port out at the same time during the surgery because I was done with treatment and I was declared that I had no evidence of the disease so my oncologist said to go on ahead and get my port removed as well. The mood was definitely a lot different for this surgery versus my LAR surgery. I was excited to go in for this surgery because I couldn’t wait to get that ileostomy reversed. The couple of weeks leading up to this surgery, the skin around my stoma was starting to get really red and irritated and I just didn’t really put a whole lot of effort into trying to figure out how to fix it because I knew that the ileostomy was going to be reversed. So I just got a prescription powder to put on the redness and sucked it up while I waited for that reversal surgery.
around my stoma was starting to get really red and irritated and I just didn’t really put a whole lot of effort into trying to figure out how to fix it because I knew that the ileostomy was going to be reversed. So I just got a prescription powder to put on the redness and sucked it up while I waited for that reversal surgery.
Surgery itself took about two hours and then I was taken to the post-anesthesia care unit, also known as the PACU, to wake up before I got sent to my hospital room. It took me longer to get out of the fog of anesthesia and it was making me anxious and apparently, I started freaking out because I was really disoriented, but I don’t remember any of this at all. They didn’t give John specific details as to what I was doing or saying they just told them that they were going to hold me in the PACU for a little bit longer while they made sure that I was calm before bringing me up to my room.
I was immediately allowed to start on the clear liquids diet once I was up, so that meant it was time to start on the jello and vegetable broth diet. I was being given Tylenol to manage my pain, but the pain was much more  tolerable than with my LAR surgery. It was only like a two or three on the pain scale. Maybe because they just had to sew the hole in my small intestine up and basically just shove it back inside of me, and then take my port out. The hole where they put the stoma back into me, they didn’t even sew that shut they just packed it with gauze and then loosely covered it with a bandage. the port scar is pretty gnarly looking as you can see from this picture I thought it looked like I had lips on my chest and, even to this day, the scar is still pretty big and noticeable. Let me show you. Here’s what it looks like.
tolerable than with my LAR surgery. It was only like a two or three on the pain scale. Maybe because they just had to sew the hole in my small intestine up and basically just shove it back inside of me, and then take my port out. The hole where they put the stoma back into me, they didn’t even sew that shut they just packed it with gauze and then loosely covered it with a bandage. the port scar is pretty gnarly looking as you can see from this picture I thought it looked like I had lips on my chest and, even to this day, the scar is still pretty big and noticeable. Let me show you. Here’s what it looks like.
I was able to move around in my bed and even get up and walk on that first afternoon in the evening. I was really pleased with how much easier this surgery was and hoped that that meant that I was going to be able to get home much faster. The next morning around 5 am I passed my first fart out of my butt in months. Passing gas is that first step in showing that your bowels are waking up and working, so I was upgraded to the full liquids diet for breakfast, and then got moved up to the soft foods diet for lunch. I spent the day just walking the halls because walking is supposed to wake your bowels up faster than just lying in bed. Plus, since I wasn’t really in a whole lot of pain, I didn’t want to just lay in bed anyway since there wasn’t anything else to do other than watch tv or walk. I also started having some mucus leak out of me and got a spot or two on the chucks pad on my bed and messed up one of my pairs of underwear. So then I switched over to wearing the adult diapers.
breakfast, and then got moved up to the soft foods diet for lunch. I spent the day just walking the halls because walking is supposed to wake your bowels up faster than just lying in bed. Plus, since I wasn’t really in a whole lot of pain, I didn’t want to just lay in bed anyway since there wasn’t anything else to do other than watch tv or walk. I also started having some mucus leak out of me and got a spot or two on the chucks pad on my bed and messed up one of my pairs of underwear. So then I switched over to wearing the adult diapers.

Wednesday morning I had my first bowel movement and it seemed normal. But in anticipation of the rest not being very normal coming very soon, I made sure to put some diaper rash cream on my butt to protect it. Having a bowel movement meant that I could be discharged, so I was super excited about that. To prep me for going home, first they took the gauze out of my stoma hole wound at about 7:30 a.m then by 9 a.m it was completelyclosed up already. It was really weird. Here’s the picture progression. I believe they leave it open and let it close itself up because if there’s any little traces of bacteria they want it open so that as it closes up it kind of pushes that out instead of having it sealed or having

it sewn shut and the bacteria is trapped inside. My surgeon’s directions for eating once I got home was to just eat like normal, no diet restrictions at all. My follow-up appointment with him was scheduled for two weeks from that discharge date and he said that he wanted to give my bowels time to adjust and regulate to being normal again and didn’t want me taking any kind of medications to regulate them for at least a month.
Once I got home though, that’s when the literal poop storm began and all hell broke loose. Anytime I stood up, it felt like all the waste inside of me just rushed down immediately and I had to hurry as fast as I could to get to the bathroom to let it out.
Once I was on the toilet though, not a whole lot came out. It felt like more needed to come out but nothing ever did. Every bowel movement was a six on the Bristol scale. If you’re unfamiliar with the Bristol scale, it’s a chart that rates your bowel movements. Let me show you the chart. A four is the normal that you want to strive for. One and two on the scale mean that you’re constipated, a six or a seven are considered diarrhea.
The first few days were spent just lying around on the couch because anytime I stood up I had that feeling that everything in me was rushing out and I would have to go to the bathroom. Even when I was lying on the couch though all day I still had almost a constant feeling that I needed to go and pass a bowel movement. I tried to hold it for as long as I could before going to the bathroom in an attempt to try and retrain my bowels so that they weren’t sending me those signals that I needed to go constantly. This wasn’t anything that a doctor told me it was just something that in my head I thought maybe would help. Instead of wearing an adult diaper I switched to wearing pads and just positioned them to the back end of my underwear to catch any leaks. I never had any like full out accidents so the pads were plenty good enough to just catch the little bit that would leak out occasionally. I didn’t count how many times I was going to the bathroom those first couple of days.
But by Saturday I was going so much I decided that I needed to track this so that I had actual data to give my doctor when I went in for my follow-up appointment rather than just saying “I’m going all the time,” I would have an exact number to tell him “I went this many times on these days.” I downloaded the My Symptoms tracker onto my phone and in that, you can keep track of your food, medications that you take, uh you can also track your bowel movements, where they fell on the Bristol scale, and also even track how urgent those movements are on a scale from zero to ten. Before I go through that tracker with you let me quickly tell you that before cancer I would usually have one bowel movement a day, it would be a four on that Bristol scale and I’d be in and out of the bathroom within five minutes.
you can keep track of your food, medications that you take, uh you can also track your bowel movements, where they fell on the Bristol scale, and also even track how urgent those movements are on a scale from zero to ten. Before I go through that tracker with you let me quickly tell you that before cancer I would usually have one bowel movement a day, it would be a four on that Bristol scale and I’d be in and out of the bathroom within five minutes.

So here’s what Saturday looked like. I had a total of nine bowel movements but I’m almost positive that I didn’t start tracking them until after lunch so I’m sure there was at least one or two before that very first one right before lunchtime. As you can see, the urgency was pretty high all afternoon and into the evening. The bathroom visits did not let up overnight on Saturday  night so as you can see I didn’t really get a whole lot of sleep that night. You know how much your butt hurts after just like one or two episodes of diarrhea? Well imagine that, but going like 10+ times a day. That’s basically what I was experiencing.
night so as you can see I didn’t really get a whole lot of sleep that night. You know how much your butt hurts after just like one or two episodes of diarrhea? Well imagine that, but going like 10+ times a day. That’s basically what I was experiencing.
My butt was getting really raw and it was burning every time that I was going even though I  was putting diaper rash cream on after every visit to the bathroom. I felt like I basically lived on the toilet on Sunday with a total of 17 visits, and almost all of them were urgent but it did let up for Sunday night so that I could get some sleep. Sunday was also the first day that I saw my first fives on the Bristol scale, so we had moved from a six to a five so there was a little bit of good news there. Monday I had 12 bowel movements that were pretty much looking like peas and marbles, and my butt was so raw the diaper rash cream wasn’t helping at all anymore. I used some Dermoplast on my butt to try and cool it off a little bit but since I was going to the bathroom basically like every hour it wasn’t really working for very long.
was putting diaper rash cream on after every visit to the bathroom. I felt like I basically lived on the toilet on Sunday with a total of 17 visits, and almost all of them were urgent but it did let up for Sunday night so that I could get some sleep. Sunday was also the first day that I saw my first fives on the Bristol scale, so we had moved from a six to a five so there was a little bit of good news there. Monday I had 12 bowel movements that were pretty much looking like peas and marbles, and my butt was so raw the diaper rash cream wasn’t helping at all anymore. I used some Dermoplast on my butt to try and cool it off a little bit but since I was going to the bathroom basically like every hour it wasn’t really working for very long.
Tuesday I started the day with two bowel movements before breakfast, another four before lunch, and my butt just couldn’t take anymore, so I turned to the internet to see if I could get any ideas of anything that I could do at home that didn’t involve medication to help me. The overall consensus was that my surgeon was crazy for telling me to just eat a normal diet and that most other people had been told to eat a low-residue diet when they came home from their ileostomy reversal surgery. So what exactly is the low-residue diet? It basically limits the amount of high fiber foods that you eat such as like whole-grain cereals, whole-grain breads, nuts, seeds, raw fruits, raw veggies with the goal of you having fewer bowel movements and smaller bowel movements. What you want to do is look for foods that have one gram of fiber or less per serving. This diet is only meant to be followed temporarily because it’s really hard to meet all your dietary needs on it.
So what foods can you eat? White bread, white pasta, refined cereals, canned fruits and vegetables, milk and foods made from milk like cheese and yogurt, tender meats, eggs, tofu, butter, margarine, and dressings without seeds. You want to make sure that the foods that you cook they’re soft and they’re tender. And you also want to make sure that you drink plenty of water so that you don’t get constipated. I sent my parents to the grocery store Tuesday afternoon with a list of all of the stuff on the low-residue diet so that they could buy me stuff and I could get started with this diet ASAP. It did help some because Wednesday and Thursday I only had eight trips to the bathroom on each day and I was brave enough to go outside and walk up and down my street so that I was still close by in case I did get an urgent feeling to go I was close enough to a toilet.
vegetables, milk and foods made from milk like cheese and yogurt, tender meats, eggs, tofu, butter, margarine, and dressings without seeds. You want to make sure that the foods that you cook they’re soft and they’re tender. And you also want to make sure that you drink plenty of water so that you don’t get constipated. I sent my parents to the grocery store Tuesday afternoon with a list of all of the stuff on the low-residue diet so that they could buy me stuff and I could get started with this diet ASAP. It did help some because Wednesday and Thursday I only had eight trips to the bathroom on each day and I was brave enough to go outside and walk up and down my street so that I was still close by in case I did get an urgent feeling to go I was close enough to a toilet.
Then Thursday I started having poop that was a number four on the Bristol scale. Friday the urgency of my visits started going down by a lot too. There were still some that were urgent but I felt like I was finally making some progress. Saturday the number of visits went back up to 16, but they were pretty much all a number four on the Bristol scale, and I believe part of the reason I went so many times was because when I was in the bathroom just to urinate I would also just pass a little bit of stool also.
Then on Monday, I started to get nervous about having to go to my surgeon the next day for my follow-up appointment. The drive to his office was about 20 minutes and I was really nervous about making it to and from his office without pooping myself. Then Tuesday came and I surprised myself and made it to and from the office without an accident. During the appointment, my surgeon looked at the ileostomy wound site and said everything looked like it was healing just fine. Then he asked how my bathroom visits were. I told him it was really bad and painful and that I started a low-residue diet the week before to try and slow things down and to let my burning butt heal. He got mad at me for restricting my diet and said he would start me on some medications so that I could get back to eating a normal diet. He said that I could take Metamucil to bulk up my stools and I could take one Imodium daily to slow them down. But he didn’t tell me to avoid taking them at the same time.
and said he would start me on some medications so that I could get back to eating a normal diet. He said that I could take Metamucil to bulk up my stools and I could take one Imodium daily to slow them down. But he didn’t tell me to avoid taking them at the same time.
After a few weeks of taking both of them, I found out that you’re not supposed to take any medications within two hours of taking the Metamucil because the Metamucil can reduce the efficacy of those medications. I took them both together that afternoon for the first time and I saw an immediate improvement in the urgency of my bathroom visits. I was still going a lot but by the next day I no longer had diarrhea and all of my bowel movements were fours or fives and I even had a three in there.
Wednesday night my sister and her husband flew into town to visit and by Thursday I was out on the town taking them around to all the touristy spots. I had nine bowel movements that day, but they looked normal and the urgency didn’t disrupt any of our activities that day. Then Sunday I was able to ride in the car for over an hour to take our daughter, Maelle to an overnight camp and I survived the ride back home without feeling like I needed to go urgently and without having an accident. Exactly three weeks from my surgery day I felt like I had improved enough that I no longer needed to track my bowel movements. I wasn’t completely back to my pre-cancer normal but my butt was healing, it wasn’t burning anymore, and I was confident enough to leave the house without being afraid of having an accident.
Exactly eight weeks after my reversal surgery I participated in Fight Colorectal Cancer’s  Climb for a Cure and hiked for over eight hours on a mountain and only pooped once during that entire hike. That was a HUGE victory for me only having gone to the bathroom one time in eight hours. There would still be bad days but I wasn’t confined to a couch anymore and I felt like I had more control over when I actually needed to go.
Climb for a Cure and hiked for over eight hours on a mountain and only pooped once during that entire hike. That was a HUGE victory for me only having gone to the bathroom one time in eight hours. There would still be bad days but I wasn’t confined to a couch anymore and I felt like I had more control over when I actually needed to go.
Have more questions about how the reversal recovery process goes? Catch me live on YouTube on Thursday, September 17th at 12 p.m. Mountain Time. I’ll be on for about an hour answering all the questions that you have about the ileostomy reversal process and how things are going now. Make sure that you’ve clicked on the subscribe button and the notifications you’re getting all of them so you’ll be notified when I do go live and when all my future videos are posted. I hope to see a bunch of you on Thursday when I go live. Thank you for watching.
*This video was originally published on September 11, 2020