
Week 1 with an Ileostomy: Eating, Emptying, and More
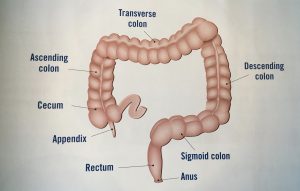
Welcome to Life as a Cancer Survivor. Jelena here, and today I’m gonna talk to you about what it’s like during that first week having an ileostomy. I had mine for seven and a half months while my bowels recovered from having a Lower Anterior Resection, which is where
they took out 12 inches of my colon/rectum and also 17 lymph nodes. I
had that surgery in October of 2016 which was five months after I was
diagnosed with Stage 3 Rectal Cancer or for those of you in Canada, Australia, or the UK, it’s Stage 3 Bowel Cancer. I have an exciting announcement to make at the end of the video so make sure that you stay tuned.
First, let me briefly describe what an ileostomy is for those of you that might be unfamiliar. It’s where they take the end of your small intestine and pull it out of your abdominal wall. We’ll say this is your small intestine, so they cut a slit in it, and then your waste will come out of your slit out of the slit and you wear a bag over your abdomen to catch that waste. So it comes out of there instead of continuing through your digestive system and coming out of your butt. If you need a more in-depth explanation, I did a video on what the ileostomy, the colostomy, and urostomies are, so click up here, I’ve got that link so you can familiarize yourself a little bit more with those. If you click on that, make sure that you come back over here and watch this video when you’re all done.
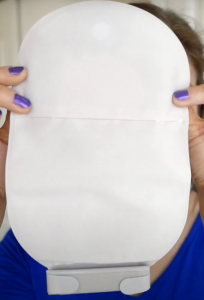
Now that you understand a little bit better what ileostomy is I’ll begin my story with when I woke up in the hospital with the bag on. So when I woke up and I looked and I saw the bag on my stomach it really started sinking in that that was gonna be a part of me for the next few months. The bag that had been placed on me was clear on the outside so you could see the output that was coming out and also the stoma. Mine it was still pretty swollen and red so it kinda looked like a big cherry to me. I’d heard from others that some people will name their stoma to kind of make it seem a little less scary, kind of gives it a little bit of a lighter side that you can laugh at, and also when it starts having a mind of its own and acting up you’ve got a name that you can call it. So since I thought it looked like a huge cherry I decided to name mine Cherries Jubilee or Juby for short. Let me know in the poll up here if you had or have a stoma, did you name it? And if you’re feeling brave go on in the comments below and let us know what you did name it.
my story with when I woke up in the hospital with the bag on. So when I woke up and I looked and I saw the bag on my stomach it really started sinking in that that was gonna be a part of me for the next few months. The bag that had been placed on me was clear on the outside so you could see the output that was coming out and also the stoma. Mine it was still pretty swollen and red so it kinda looked like a big cherry to me. I’d heard from others that some people will name their stoma to kind of make it seem a little less scary, kind of gives it a little bit of a lighter side that you can laugh at, and also when it starts having a mind of its own and acting up you’ve got a name that you can call it. So since I thought it looked like a huge cherry I decided to name mine Cherries Jubilee or Juby for short. Let me know in the poll up here if you had or have a stoma, did you name it? And if you’re feeling brave go on in the comments below and let us know what you did name it.
Once I started getting some output I asked the nurse what I should do as it started filling up. So she said to use the call button on my remote and either the nurse or the CNA which is the Certified Nursing Assistant, would come down and they would empty it for me because they were keeping track of the output so they would actually empty it into a plastic
container that had measurements on it so that they could note how much output I had. For the first couple of days, the output was just liquid and I was really glad that I did not have to deal with it ’cause it was pretty gross. The day came that I was gonna be discharged from the hospital and I had to do a bag change before I left. I was pretty nervous about doing it. I wasn’t sure how I was gonna react to seeing the stoma all by itself without the bag on it. I wasn’t even exactly sure how the small intestine was coming out of me, so I didn’t know if I was even gonna be able to look at it and figure out what exactly was going on without being completely grossed out, but I was about to find out shortly.
pretty gross. The day came that I was gonna be discharged from the hospital and I had to do a bag change before I left. I was pretty nervous about doing it. I wasn’t sure how I was gonna react to seeing the stoma all by itself without the bag on it. I wasn’t even exactly sure how the small intestine was coming out of me, so I didn’t know if I was even gonna be able to look at it and figure out what exactly was going on without being completely grossed out, but I was about to find out shortly.
Once the wound care nurse came up to my room to help me with my bag change, she kind of settled my fears a little bit by showing me some
tips like taking a washcloth and tucking it in like a bib but in your underwear so that any output that may leak out you’ve got that washcloth there handy to wipe up any spills. She scheduled her visit with me for about two hours after breakfast in hopes that my stoma would be pretty quiet and there wouldn’t be a whole lot of output when we were doing the change. She ended up pretty much doing most of the bag change herself as I kind of assisted a little and just kind of watched, tried to take notes in my head but it was pretty overwhelming. She reassured me though that I would have a home health nurse that would come visit me for two weeks and that nurse would help me at home with the changes, so if I didn’t remember everything, that nurse at my house would be able to help me remember those and help me get kind of a rhythm down. Then she gave me some supplies to take home with me to keep me held over for a few weeks while I requested samples from the three major ostomy supply companies Convatec, Hollister, and Coloplast.
with me for about two hours after breakfast in hopes that my stoma would be pretty quiet and there wouldn’t be a whole lot of output when we were doing the change. She ended up pretty much doing most of the bag change herself as I kind of assisted a little and just kind of watched, tried to take notes in my head but it was pretty overwhelming. She reassured me though that I would have a home health nurse that would come visit me for two weeks and that nurse would help me at home with the changes, so if I didn’t remember everything, that nurse at my house would be able to help me remember those and help me get kind of a rhythm down. Then she gave me some supplies to take home with me to keep me held over for a few weeks while I requested samples from the three major ostomy supply companies Convatec, Hollister, and Coloplast.
 You can’t really ask for samples ahead of time because you don’t know what the size of your stoma is gonna be, and the size of your stoma is gonna determine what size barrier you’re gonna need which this is the part that sticks on to you so your stoma sticks out the hole. You can cut them, but some are larger than others and then depending on what size of the barrier you get the bags that fit onto it only fit on certain sized barriers so you can’t even order half of it ahead of time because you got to know what size the stoma is. And even once you do order stuff, don’t order a ton initially because your stoma is still gonna change sizes for at least that first month that you’re at home.
You can’t really ask for samples ahead of time because you don’t know what the size of your stoma is gonna be, and the size of your stoma is gonna determine what size barrier you’re gonna need which this is the part that sticks on to you so your stoma sticks out the hole. You can cut them, but some are larger than others and then depending on what size of the barrier you get the bags that fit onto it only fit on certain sized barriers so you can’t even order half of it ahead of time because you got to know what size the stoma is. And even once you do order stuff, don’t order a ton initially because your stoma is still gonna change sizes for at least that first month that you’re at home.
Once I got home I was really nervous about eating. The nurses at the hospital had really emphasized that I needed to chew VERY thoroughly all of the food that I was eating once I got home and that I needed to avoid any high-fiber foods for at least six weeks after surgery because those foods take a lot more work to digest and my digestive system had already been traumatized enough from surgery it didn’t need to be
overworked by trying to digest those foods as well. So, more specifically those high-fiber foods that I was supposed to avoid eating were: whole-wheat breads, brown rice, raw fruits and vegetables, and dried fruit. 
I was also given a list of foods that I was supposed to avoid for the first six weeks after surgery to help avoid or decrease the chance of me getting an intestinal blockage. Those foods are:
- vegetable and fruit skins
- apples, dried fruit, grapes, coconut, and pineapple
- celery, corn, cucumber, green peppers, peas, and bean sprouts
- salad greens, cabbage, coleslaw, and spinach
- nuts
- casings on sausage and tough, fibrous meats like steaks
I passed these lists on to my parents because they were gonna be making meals for us for the first bit after I got home from surgery. So the first meal that they prepared for us for that dinner was a creamy potato soup, with the potatoes peeled. It took me forever to eat because I chewed so thoroughly I probably spent a minute on each bite before I swallowed it. Luckily I guess I wasn’t eating a whole lot so even though I was taking me forever to eat each bite I still finished around the same time as everybody else because they were eating a little bit more than I was.
Once I got home I had to figure out how I was gonna empty my ostomy bag. At the hospital, they just emptied it into a plastic measuring container while I was still sitting at the hospital bed. At home, I would be
emptying it while I was on the toilet. So there are a couple of different methods that you can choose from for emptying your bag:
Forward Method – you sit on the toilet like you normally would and empty your bag.

The Backward Method – is where you sit on the toilet facing the tank and empty.
The Kneeling Method – is when you kneel on the floor either in front or to the side of the toilet and empty.
You can also put a few squares of toilet paper on top of the water in the bowl to help try and prevent some splashage while you’re emptying the bag. Then after you’ve emptied the bag I would take a little toilet paper and I would wipe the outside and the inside of the end a little bit so that when I folded it up there wasn’t any waste that was squishing out of it then I would fold it up and be on my way.
I experimented with using my old peri bottle, which was a squirt bottle that you get after you’ve given birth to kind of hose yourself off after you’ve used the bathroom. So I had that squirty bottle and I would try
that you get after you’ve given birth to kind of hose yourself off after you’ve used the bathroom. So I had that squirty bottle and I would try
rinsing out the bag after emptying it but the water would feel really cold if you didn’t fill it up with warm water (right away) right before you went. And then it’s just swirling around poop all over and it was really hard to get it completely clean and within like five minutes it’s dirty again. So it wasn’t really worth it, and then I also read that it can loosen up some of the adhesive and cause your barrier to break down faster so that was kind of the final straw for me and I decided trying to rinse out the bag was not worth it.
I preferred the forward method because I would always pee when I emptied my bag and it was just easier to empty it in the position that I was already in on the toilet. I was told to never let the waste get more than about halfway up in your ostomy bag before you empty it, I believe for two reasons. One is because you don’t want that waste getting backed up so high that it’s resting on your stoma. Especially with the ileostomy because the waste coming out of your ileostomy is more acidic than regular stool so it could cause burns, especially around where the barrier is surrounding your stoma and it could break that down much quicker when there’s stool just resting on it. Also, when it gets more than half-full that bag gets pretty heavy, and even if it’s not peeling off, having that stress is gonna cause the adhesive on the barrier to break down faster.
 I tried to drink a lot of water while I had my ileostomy because your large intestine is what is absorbing most of the liquid for your body, and since that wasn’t in use and it was coming out of the small intestine I needed to drink more water to make sure that I didn’t get dehydrated. So since I was drinking more water I was peeing a lot more which gave me a lot of opportunities to empty that bag.
I tried to drink a lot of water while I had my ileostomy because your large intestine is what is absorbing most of the liquid for your body, and since that wasn’t in use and it was coming out of the small intestine I needed to drink more water to make sure that I didn’t get dehydrated. So since I was drinking more water I was peeing a lot more which gave me a lot of opportunities to empty that bag.
Two days after I got home from the hospital I had my first visit from the home health nurse and did my first bag change at home. Getting the bag off was a piece of cake. Getting it back on was a different story. My tummy was still really sore and my muscles were a wreck from surgery. When you’re trying to click the bag onto the barrier you need some kind of resistance on the barrier side to allow that click to happen, but my
muscles were shot and I couldn’t flex my muscles at all to give any kind of resistance. I kept trying and trying and trying to get it to click but I couldn’t get it to click. In between attempts, poop was coming out so I had to keep cleaning it up. After like five minutes of struggling I still hadn’t got it on so the nurse decided to try and do it. The nurse tried to get that bag to click on too and she even struggled. She worked up a sweat trying to get it on but finally, she got it on. It was a disaster. I was really frustrated once the visit was over and really fearful for how I was ever gonna change my bag on my own.
The next visit wasn’t a whole lot better. We tried connecting the barrier and the bag together first before putting it on me, but my stoma wasn’t perfectly round so it’s really hard to get it perfectly lined up. So we got it on but it wasn’t perfect, so a little bit of my skin was showing and the part that was showing ended up getting burned by the output.
The first week with an ileostomy was a struggle. I even knew going into surgery that I was gonna get one and it was still hard for me. Beyond getting marked for the stoma and just seeing a basic demonstration on a dummy of how to put a bag on, I didn’t really know what I was in store for. Changing that bag was SO hard. I was so sore too, that all I could wear were sweat pants, really loose-fitting elastic waist banded pants, and flowy shirts.
into surgery that I was gonna get one and it was still hard for me. Beyond getting marked for the stoma and just seeing a basic demonstration on a dummy of how to put a bag on, I didn’t really know what I was in store for. Changing that bag was SO hard. I was so sore too, that all I could wear were sweat pants, really loose-fitting elastic waist banded pants, and flowy shirts.
One more thing that I want to share with you all is that I’m launching website, Life as a Cancer Survivor! Over there I will have the subtitles to all of my YouTube videos so that you can go back and reference them in print. I don’t have all of them up quite yet but they should be finished within the next few weeks. I’ll also have a list of my favorite resources and then I’ll also have a timeline of my diagnosis and treatment for you to look at. If there’s anything else that you would like to hear from me
or see on the website, just let me know. Drop me a line in the comments and I’ll look into getting that added.
There is plenty more that I want to share with you about what it’s like living with an ileostomy and I couldn’t fit it all in this video, so make sure that you’re subscribed and that you’ve clicked on the bell so you’re notified when all of my future videos are posted. My channel is growing and it’s thanks to the love that each of you are giving to this channel.
Thank you so much for watching and I’ll see you again soon.
*This video was originally published on June 19, 2020























 afternoon the nurse from the oncologist’s office called me to give me instructions on how to take them. She said don’t crush them up and to try as hard as I could to take the dosage 12 hours apart, once in the morning and once in the evening. She also made sure that I knew that I was only supposed to be taking those pills on the days I went in for radiation, so Monday through Friday. I took two pills in the morning and then three pills in the evening 12 hours later. I’m not sure how well you can tell the size of them from this picture but here’s a picture of them next to a juice glass from my last week of chemo.
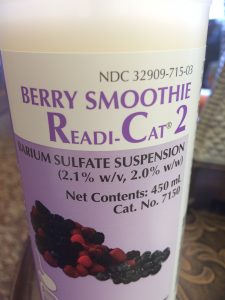
afternoon the nurse from the oncologist’s office called me to give me instructions on how to take them. She said don’t crush them up and to try as hard as I could to take the dosage 12 hours apart, once in the morning and once in the evening. She also made sure that I knew that I was only supposed to be taking those pills on the days I went in for radiation, so Monday through Friday. I took two pills in the morning and then three pills in the evening 12 hours later. I’m not sure how well you can tell the size of them from this picture but here’s a picture of them next to a juice glass from my last week of chemo. June 13th was my first day of radiation and oral chemotherapy and I also had my MRI scheduled for that day. I woke up at 5:45 a.m. to eat a muffin and take the first dose of chemotherapy pills to give me six hours between then and when I was scheduled to be at the hospital for my MRI. I was supposed to check-in at 12:15pm for that MRI at the hospital so if I woke up at 5:45 ate breakfast and the chemo pills I’d be done by 6:15 for sure and that would give me the six hours I needed to fast before the MRI. I tried to go back to sleep but I couldn’t fall asleep I started dozing off once everyone else started waking up so I just got up.
June 13th was my first day of radiation and oral chemotherapy and I also had my MRI scheduled for that day. I woke up at 5:45 a.m. to eat a muffin and take the first dose of chemotherapy pills to give me six hours between then and when I was scheduled to be at the hospital for my MRI. I was supposed to check-in at 12:15pm for that MRI at the hospital so if I woke up at 5:45 ate breakfast and the chemo pills I’d be done by 6:15 for sure and that would give me the six hours I needed to fast before the MRI. I tried to go back to sleep but I couldn’t fall asleep I started dozing off once everyone else started waking up so I just got up. halfway through my treatment. She made it sound like nobody had ever asked that before which I find suspicious, but she said as long as it was in moderation I was okay. Then she went over a list of all the possible side effects of chemotherapy and she even gave me a nice handout that broke it all down based on how common all of the side effects were. She said that the main side effects that most people experience while on Xeloda at varying degrees of severity are more than 25% of patients experience the side-effect of Hand-Foot Syndrome which includes redness and swelling of the hands and feet which can prevent normal activity, cracking and peeling of skin on the hands and feet, and then tingling and numbness or burning again in the hands and feet. Diarrhea was also a common side effect which includes cramping, gas, and bloating which I experienced the diarrhea and the cramping but I’m not sure if it was from the radiation or from the chemotherapy or both of them since I was taking them at the same time.
halfway through my treatment. She made it sound like nobody had ever asked that before which I find suspicious, but she said as long as it was in moderation I was okay. Then she went over a list of all the possible side effects of chemotherapy and she even gave me a nice handout that broke it all down based on how common all of the side effects were. She said that the main side effects that most people experience while on Xeloda at varying degrees of severity are more than 25% of patients experience the side-effect of Hand-Foot Syndrome which includes redness and swelling of the hands and feet which can prevent normal activity, cracking and peeling of skin on the hands and feet, and then tingling and numbness or burning again in the hands and feet. Diarrhea was also a common side effect which includes cramping, gas, and bloating which I experienced the diarrhea and the cramping but I’m not sure if it was from the radiation or from the chemotherapy or both of them since I was taking them at the same time. By the final week of taking the pills the only side effect that I was feeling that I could definitely attribute to the Xeloda was the Hand-Foot Syndrome. It wasn’t as severe as others have gotten it but my hands and feet were red and it was really painful to walk or even stand on my feet. My appetite was pretty low by that last week too. I discovered that if I took the Zofran, even though I wasn’t feeling nauseous taking that did help increase my appetite a little bit. But the side effect from that is that it would constipate me.
By the final week of taking the pills the only side effect that I was feeling that I could definitely attribute to the Xeloda was the Hand-Foot Syndrome. It wasn’t as severe as others have gotten it but my hands and feet were red and it was really painful to walk or even stand on my feet. My appetite was pretty low by that last week too. I discovered that if I took the Zofran, even though I wasn’t feeling nauseous taking that did help increase my appetite a little bit. But the side effect from that is that it would constipate me.
 cancer was we learned that it was Stage 3 Rectal Cancer and that the first step in my treatment was going to be 28 days of radiation therapy and oral chemotherapy. I’ll have the links to the
cancer was we learned that it was Stage 3 Rectal Cancer and that the first step in my treatment was going to be 28 days of radiation therapy and oral chemotherapy. I’ll have the links to the  tumor was, where exactly it was located so he knew he was working off of correct information. He said that the EUS or that rectal ultrasound measured the tumor ranging from four and a half centimeters in, to 15 centimeters in. For us Americans that means the tumor was over four inches long which is like the size of an apple! That sounded huge.
tumor was, where exactly it was located so he knew he was working off of correct information. He said that the EUS or that rectal ultrasound measured the tumor ranging from four and a half centimeters in, to 15 centimeters in. For us Americans that means the tumor was over four inches long which is like the size of an apple! That sounded huge. waiting for my radiation treatment every day. I even got my own special card with a barcode on it so I could beep past that first waiting area and go to the second one. And on the back of this I stuck a picture of Maelle so she could be with me for all of my treatments. On the way down to the room, they showed me the nurse’s station where they would be watching me from for my treatments. Obviously they weren’t allowed to be in the room with me, so there were monitors that had a direct feed of video into the radiation room so they could watch and make sure everything was going as planned in there and then it also had the CT scan of me and then just a couple of other monitors up there.
waiting for my radiation treatment every day. I even got my own special card with a barcode on it so I could beep past that first waiting area and go to the second one. And on the back of this I stuck a picture of Maelle so she could be with me for all of my treatments. On the way down to the room, they showed me the nurse’s station where they would be watching me from for my treatments. Obviously they weren’t allowed to be in the room with me, so there were monitors that had a direct feed of video into the radiation room so they could watch and make sure everything was going as planned in there and then it also had the CT scan of me and then just a couple of other monitors up there. staying on and things getting erased so I just went for the permanent tattoo. They did it right there on the table they just came in with a needle of ink stuck the needle in and just injected the ink and it’s about the size of a freckle but visible enough as you can see.
staying on and things getting erased so I just went for the permanent tattoo. They did it right there on the table they just came in with a needle of ink stuck the needle in and just injected the ink and it’s about the size of a freckle but visible enough as you can see. picture of me, then they went back to the waiting room while I hopped up on the table for treatment. As I mentioned earlier, I had to lay face down for treatment and then I had to pull my pants and my underwear down to my knees. The nurses would hang a towel over my butt so it wasn’t hanging out the whole time, but then they’d tape my butt cheeks apart so that the radiation wouldn’t build up even more and cause worse burns in any folds back there.
picture of me, then they went back to the waiting room while I hopped up on the table for treatment. As I mentioned earlier, I had to lay face down for treatment and then I had to pull my pants and my underwear down to my knees. The nurses would hang a towel over my butt so it wasn’t hanging out the whole time, but then they’d tape my butt cheeks apart so that the radiation wouldn’t build up even more and cause worse burns in any folds back there.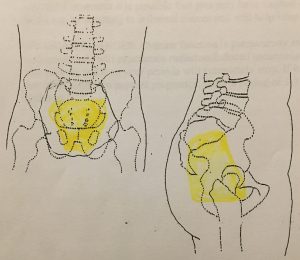 to be treated with radiation. My appointments are scheduled for 15 minutes each day but most of that 15 minutes is spent getting me all perfectly lined up on the table so that they don’t accidentally zap the wrong parts of me during radiation.
to be treated with radiation. My appointments are scheduled for 15 minutes each day but most of that 15 minutes is spent getting me all perfectly lined up on the table so that they don’t accidentally zap the wrong parts of me during radiation. getting so bad it was waking me up in the middle of the night. I was also having bad cramping episodes that would just kind of lay me out on the couch for hours at a time. Week 2 was also when my appetite started to decrease. By the end of the week I had almost a constant feeling of needing to go to the bathroom all the time, but when I would go and try to push something out just blood would come out into the toilet. My pain would rotate through cramps, gas, feeling like I needed to go to the bathroom all the time, and just like my rectum felt sore all the time. The sore rectum was pretty much a constant but those others kind of rotated sometimes would last just for a few minutes other times up to an hour. They would happen often enough that I didn’t feel comfortable going out for a hike or being away from a bathroom for very long.
getting so bad it was waking me up in the middle of the night. I was also having bad cramping episodes that would just kind of lay me out on the couch for hours at a time. Week 2 was also when my appetite started to decrease. By the end of the week I had almost a constant feeling of needing to go to the bathroom all the time, but when I would go and try to push something out just blood would come out into the toilet. My pain would rotate through cramps, gas, feeling like I needed to go to the bathroom all the time, and just like my rectum felt sore all the time. The sore rectum was pretty much a constant but those others kind of rotated sometimes would last just for a few minutes other times up to an hour. They would happen often enough that I didn’t feel comfortable going out for a hike or being away from a bathroom for very long. slower and with the gas pains that were plaguing me and the blood that was passing with the gas, it made it really difficult to run. On my last radiation day, I got this cool certificate and I also got to ring the bell to signify that I was finished with radiation.
slower and with the gas pains that were plaguing me and the blood that was passing with the gas, it made it really difficult to run. On my last radiation day, I got this cool certificate and I also got to ring the bell to signify that I was finished with radiation.
 But as a stay-at-home mom with a five-year-old that worked part-time from home, it was going to be really hard to hide all the tests and treatments from her. So we wanted to let her know what was going on early on in the process as soon as we knew what was going to happen. The question would be, how would she handle the news as a five-year-old?
But as a stay-at-home mom with a five-year-old that worked part-time from home, it was going to be really hard to hide all the tests and treatments from her. So we wanted to let her know what was going on early on in the process as soon as we knew what was going to happen. The question would be, how would she handle the news as a five-year-old? I’m sure her little brain was just grinding away trying to figure out and process all that we had just told her.
I’m sure her little brain was just grinding away trying to figure out and process all that we had just told her. I think having my parents come and stay with us for those first three weeks obviously really helped in many ways, but also really helped to serve as a great distraction for Maelle. It gave her two people to play with, which was really important since she was an only child and there weren’t really any young kids in our neighborhood. But it also freed me up to be able to go into my daily treatments without having to drag her with me.
I think having my parents come and stay with us for those first three weeks obviously really helped in many ways, but also really helped to serve as a great distraction for Maelle. It gave her two people to play with, which was really important since she was an only child and there weren’t really any young kids in our neighborhood. But it also freed me up to be able to go into my daily treatments without having to drag her with me.
 The PET scan would show that indeed the lymph node, the enlarged lymph node, in my chest was not cancer but there were multiple lymph nodes involved near the rectum. Ultimately he said that his prognosis for me was that this was curable and that my worst-case scenario would be that I would have a colostomy bag for the rest of my life. Hearing the oncologist say that he believed this was curable was a huge weight lifted off of my shoulders knowing that I was gonna survive this. Curable is not a term that oncologists throw around lightly so I knew that he was confident we were gonna get rid of this nasty cancer.
The PET scan would show that indeed the lymph node, the enlarged lymph node, in my chest was not cancer but there were multiple lymph nodes involved near the rectum. Ultimately he said that his prognosis for me was that this was curable and that my worst-case scenario would be that I would have a colostomy bag for the rest of my life. Hearing the oncologist say that he believed this was curable was a huge weight lifted off of my shoulders knowing that I was gonna survive this. Curable is not a term that oncologists throw around lightly so I knew that he was confident we were gonna get rid of this nasty cancer. Step 2 of my treatment would be major surgery. The doctor that would be doing my surgery preferred to wait 12 weeks after finishing radiation and chemotherapy to do the surgery. He liked to wait that long because after you’re done with those the tumor continues to shrink afterwards. During that surgery, the plan was to remove enough of my colon and rectum that there were clear margins that had no cancer cells in them on either side of the tumor. They would also remove an unknown number of lymph nodes, whatever looked like they were still cancerous that were nearby the rectum. Depending on how much my tumor shrank from step 1 would determine whether or not the tumor was far enough away to save my sphincter muscles and allow me to just have a temporary ileostomy or if they would have to take all of it and I would end up with a permanent colostomy.
Step 2 of my treatment would be major surgery. The doctor that would be doing my surgery preferred to wait 12 weeks after finishing radiation and chemotherapy to do the surgery. He liked to wait that long because after you’re done with those the tumor continues to shrink afterwards. During that surgery, the plan was to remove enough of my colon and rectum that there were clear margins that had no cancer cells in them on either side of the tumor. They would also remove an unknown number of lymph nodes, whatever looked like they were still cancerous that were nearby the rectum. Depending on how much my tumor shrank from step 1 would determine whether or not the tumor was far enough away to save my sphincter muscles and allow me to just have a temporary ileostomy or if they would have to take all of it and I would end up with a permanent colostomy. surgery but was most likely gonna happen just because of my age. Step 3 would take place six to eight weeks after surgery to give my body time to recover from all that slicing and dicing and it would be eight cycles of intravenous chemotherapy called FOLFOX. They wanted to do the second round for what they called mop-up chemo. Since I was so young at diagnosis and the cancer had spread to my lymph nodes they weren’t sure if any stray cells had gotten loose and were swirling around in my lymphatic system just waiting to multiply and spread more. So to make extra sure that they killed all the cancer cells and would give me tons of cancer-free years after this they voted to go aggressive with my treatment and have me do eight cycles of chemotherapy after surgery.
surgery but was most likely gonna happen just because of my age. Step 3 would take place six to eight weeks after surgery to give my body time to recover from all that slicing and dicing and it would be eight cycles of intravenous chemotherapy called FOLFOX. They wanted to do the second round for what they called mop-up chemo. Since I was so young at diagnosis and the cancer had spread to my lymph nodes they weren’t sure if any stray cells had gotten loose and were swirling around in my lymphatic system just waiting to multiply and spread more. So to make extra sure that they killed all the cancer cells and would give me tons of cancer-free years after this they voted to go aggressive with my treatment and have me do eight cycles of chemotherapy after surgery. Step 4 would happen one to two months after my final cycle of chemotherapy if I ended up with a temporary ileostomy. I would have those 1-2 months to recover from those cycles of chemotherapy, build up my strength, build up my immune system, and they would reverse that ileostomy.
Step 4 would happen one to two months after my final cycle of chemotherapy if I ended up with a temporary ileostomy. I would have those 1-2 months to recover from those cycles of chemotherapy, build up my strength, build up my immune system, and they would reverse that ileostomy.
 endoscopic ultrasound, also known as a rectal EUS which is what I’m gonna call it for the rest of the video. Since this was another test that uses equipment that goes up your butt to check out things in there it required another colonoscopy prep. This time though I did the ironically named GoLytely prep because you certainly aren’t going lightly after you finish off that gallon jug with the powder.
endoscopic ultrasound, also known as a rectal EUS which is what I’m gonna call it for the rest of the video. Since this was another test that uses equipment that goes up your butt to check out things in there it required another colonoscopy prep. This time though I did the ironically named GoLytely prep because you certainly aren’t going lightly after you finish off that gallon jug with the powder. My final scan was a PET scan, which stands for positron emission tomography, and that was done two days after the MRI. I had to fast for six hours again before this test but this time I didn’t wake up super early in the morning to eat something I slept through the night so dinner was my last meal. When I went back for the scan they told me that the injection was sugar with a radiation tracer and that I would have to lay still in a chair for an hour while I waited for that to circulate through my body so in went yet another IV she tested it with a saline solution to make sure it was working, I got the nasty taste in the back of my throat, so she left to go get the injection.
My final scan was a PET scan, which stands for positron emission tomography, and that was done two days after the MRI. I had to fast for six hours again before this test but this time I didn’t wake up super early in the morning to eat something I slept through the night so dinner was my last meal. When I went back for the scan they told me that the injection was sugar with a radiation tracer and that I would have to lay still in a chair for an hour while I waited for that to circulate through my body so in went yet another IV she tested it with a saline solution to make sure it was working, I got the nasty taste in the back of my throat, so she left to go get the injection.