
FOLFOX Chemo Side Effects and Tips to Deal With Them
Hi everyone! In this video, I’m gonna dive deeper into the side effects that I experienced while on the IV chemotherapy FOLFOX and some tips and tricks that I either learned or figured out to help manage them. In case you’re new here, welcome to Life as a Cancer Survivor. My name is Jelena and in May of 2016 I was diagnosed with Stage 3 Rectal Cancer. This channel, I started to show you what life is like as a young Colorectal Cancer survivor and how life is both during and after treatment ends. You can also follow me and my life adventures over on either Instagram or on Twitter the handles are popping up over here but I’ll also have links that will take you directly to my profile so you can follow me down in the description below. So come on over and say, “Hi!”
I received eight rounds of the IV chemotherapy FOLFOX starting on December 13th, 2016.  Within the first hour of that infusion, the side effects started kicking in. I had been sipping my water the whole time off and on, but all of a sudden when I took a drink and I swallowed, it felt like I was swallowing glass. It really startled me and I wasn’t sure if I was just going crazy or if that actually happened so I took another sip and the same thing happened so I realized that must be the cold sensitivity that my Physician Assistant or my PA had been talking about when I went to the chemo training class and why they recommend drinking only warm beverages for those first few days at chemo and after receiving chemo.
Within the first hour of that infusion, the side effects started kicking in. I had been sipping my water the whole time off and on, but all of a sudden when I took a drink and I swallowed, it felt like I was swallowing glass. It really startled me and I wasn’t sure if I was just going crazy or if that actually happened so I took another sip and the same thing happened so I realized that must be the cold sensitivity that my Physician Assistant or my PA had been talking about when I went to the chemo training class and why they recommend drinking only warm beverages for those first few days at chemo and after receiving chemo.
I would go in for chemo on Tuesdays then usually around Saturday sometimes a day or two later, that cold sensitivity of my throat would go away by then. But in the meantime, it was warm water only for me. I usually just sip water throughout the day so I would have to keep reheating my glass of water over and over in the microwave because even at room temperature it still felt like I was swallowing glass so it had to be warm water that I was drinking. By the second or third round of chemo, the water started tasting like rubbing alcohol to me. So I had to have my husband, John, taste test it to make sure that something weird wasn’t going on with our water at our house. He said it tasted normal so it was just my tastebuds changing and causing that water to taste like rubbing alcohol.
Here are some tips and tricks that I learned or figured out to help with managing that called sensitivity in my throat and that bad water taste without overdosing on sugary drinks:
-Add some apple juice, or your favorite juice to a glass of water. I would do a mixture of about 25% juice 75% water, and that helped with taking that bad taste of the water away. On the days where you’re experiencing cold sensitivity, warm that glass up in the microwave after you’ve mixed the juice and the water together.
-Flavored sparkling water like La Croix, Bubly, or just your favorite grocery store brand of sparkling water is a good way, a good thing to drink to help keep you hydrated on those

days that you’re not experiencing the cold sensitivity but when water tastes nasty.
-Herbal tea is another beverage that you can drink either hot or cold and also you can sweeten it easily to your liking. My favorite ones are the fruit flavors Celestial Seasonings teas, but any of the fall and winter flavors of their herbal teas are also delicious.
Other cold sensitivity side effects that I experienced were, the first one was when cold wind would blow in my face it would be like a stabbing pain like needles stabbing me in the face. I would try to cover up with a hat and a scarf to hide as much of my face as possible but the wind would still sneak in somehow and I would get that needle stabbing feeling in my face. One other cold sensitivity side effect that I also experienced was I needed to wear oven mitts to grab stuff out of the refrigerator because if I touched cold things with my hands it felt like I was getting electrocuted in my hands as soon as the cold hit my hands so, the oven mitts protected me and kept that feeling of being electrocuted constantly away from my hands.
One major side effect that you’ll experience most likely no matter what chemo that you’re on  is fatigue. My Oncologist’s PA mentioned when I asked about the fatigue, she said that it was gonna be more intense than the fatigue that I felt while I was on the oral chemotherapy Xeloda the summer before. So she was definitely right. When I would come home from my infusions at the cancer center I would go straight to bed and take a nap for at least two hours and that was in like the late afternoon. Then I was still exhausted after dinner and I’d be ready for bed at like 8 o’clock in the evening, which is unusual for me because I’m usually a night person. So I would go to bed at like 8pm and I’d fall asleep for two hours or so, but then I’d wake up and I couldn’t fall back asleep and I’d be restless all night and exhausted the next day.
is fatigue. My Oncologist’s PA mentioned when I asked about the fatigue, she said that it was gonna be more intense than the fatigue that I felt while I was on the oral chemotherapy Xeloda the summer before. So she was definitely right. When I would come home from my infusions at the cancer center I would go straight to bed and take a nap for at least two hours and that was in like the late afternoon. Then I was still exhausted after dinner and I’d be ready for bed at like 8 o’clock in the evening, which is unusual for me because I’m usually a night person. So I would go to bed at like 8pm and I’d fall asleep for two hours or so, but then I’d wake up and I couldn’t fall back asleep and I’d be restless all night and exhausted the next day.
Finally at my third pre-chemo appointment with the PA I mentioned that restlessness and the horrible time I was having sleeping and the PA she was like, “Oh, that’s most likely from the Leucovorin because it’s a kind of steroid that you’re getting in your infusion so let me prescribe you some Ambien to help you with your sleep.” So she told me to just take it for those three or four days at the beginning when I was really having a lot of trouble sleeping so I did and it worked like a charm. And I didn’t get any of the bad side effects like the sleep eating or sleep-driving while I was on it and I didn’t get addicted to it either so for me it was a good solution to help me with those temporary sleep problems.
Even with the Ambien to help me with sleeping at night, I still felt fatigued on many days. The fatigue is just different from feeling tired. Even when I would get a full night’s sleep and would nap I would still feel exhausted. Taking naps or trying to get out for some exercise which usually would perk me up didn’t work at all. There wasn’t really a whole lot that I could do beyond trying to get a full night’s sleep at night to help the fatigue other than to limit the amount of energy that I put out during the day and make sure I wasn’t pushing myself too hard or doing too many things.
So one change that we did make was we moved Maelle from half-day kindergarten to full-day kindergarten so instead of us having to go get her at 11:15am, she would be at school until 3:15pm, which meant that I had a lot more time to get in those naps during the day without her being at home, and we wouldn’t have to her I wouldn’t have to hurry home after chemotherapy to pick her up at 11:15 in the morning she was at school till 3:15pm, so that was stress that was taken off of me as well. Now I just had to keep her entertained for about two hours or so after school instead of from 11:15am to 5:30pm when John came home from work.
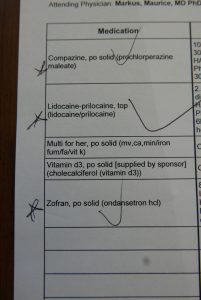
Another common side effect for anybody going through chemotherapy is nausea. I was written a prescription for two different anti-nausea meds Zofran and Compazine. The instructions I was given were on the day of chemotherapy I would usually get home early afternoon or so, I was supposed to take my first Zofran that evening and then every 8 hours for the next 2-3 days I was supposed to keep taking the Zofran. The Compazine was there in case I had breakthrough nausea or I got nauseous in between the Zofran doses I could take a dose of the Compazine to help. Well, after my first round of chemotherapy I suffered with nausea for a few days and the Compazine and Zofran didn’t really seem to help at all. I wasn’t throwing up but I didn’t have any kind of appetite and just felt nauseous. So after the second round instead of waiting until the evening to take the Zofran, I took it as soon as I got home from my chemotherapy and that seemed to work. So I just started those right away instead of waiting a few more hours which helped to kind of keep me ahead of the curve of nausea and kind of stop it before it started getting out of control. There are many other options of anti-nausea medications that you can take so if you’re struggling with nausea please talk to your oncologist and see if there are any other solutions that they have that they can that can help you.
The next side-effect that I had to deal with were muscle cramps in my hands. This would just happen while I was at chemotherapy and they would just kind of mostly tense up and it would be more difficult to try and move them like normal. I don’t really have any solutions to this but it was comforting to know at least that this was something that was going to happen and it wasn’t anything that was life-threatening just to keep me calm when it would start happening. Once the cramping went away, my hands just kind of in general were feeling weaker and even today three years later I have troubles with unscrewing lids on jars, when I’m typing I make a lot more mistakes, and even when I’m trying to play my violin moving my fingers quickly can be a struggle sometimes.
I also got neuropathy in my feet. It started out as a feeling like when you sit on your foot wrong and it falls asleep, then the feeling that I had was the part when your foot starts waking up. And that would usually only last for like a day or two but then as I moved further and further along through my rounds of chemotherapy it kind of started lasting longer and longer and by my last round of chemo, they decided to leave the Oxaliplatin out completely because that’s what causes it and they didn’t want to cause any further nerve damage.
The tingling then changed to the “my foot just fell asleep” feeling and I would only have that pins and needles tingling occasionally. I didn’t ever completely lose feeling in my feet but the
 neuropathy did make it harder for me to react quickly on my feet. I never really noticed it too much except like when we would go hiking I would feel a lot clunkier, and if I didn’t have the high-top hiking boots that I always wore there were many times where I would have snapped an ankle because I couldn’t have reacted fast enough on the rocky terrain to straighten myself up. Also when I would exercise or walk for more than a half-hour at a time, my feet would start burning. Wearing some compression socks that went over the calf did help a little bit but it didn’t completely get rid of that burning feeling. And then eventually every night when I would go to bed and lie down in bed that burning feeling would return to my feet. That’s when I decided it was time to try some acupuncture to see if that would help. It definitely wasn’t a quick fix, but I am happy to report that after two years of acupuncture treatment the tingling and burning did finally go away in my feet.
neuropathy did make it harder for me to react quickly on my feet. I never really noticed it too much except like when we would go hiking I would feel a lot clunkier, and if I didn’t have the high-top hiking boots that I always wore there were many times where I would have snapped an ankle because I couldn’t have reacted fast enough on the rocky terrain to straighten myself up. Also when I would exercise or walk for more than a half-hour at a time, my feet would start burning. Wearing some compression socks that went over the calf did help a little bit but it didn’t completely get rid of that burning feeling. And then eventually every night when I would go to bed and lie down in bed that burning feeling would return to my feet. That’s when I decided it was time to try some acupuncture to see if that would help. It definitely wasn’t a quick fix, but I am happy to report that after two years of acupuncture treatment the tingling and burning did finally go away in my feet.
One more side effect was my sense of smell got thrown off sometimes. I noticed this the worst or the most when I would shower. The water coming down on me in the shower it would smell like cooked cabbage. Multiple times I called John and had him come over and smell the water while I was in there to see if it smelled to him, but he thought it smelled like normal so it was just me and my sense of smell was off and somehow the water smelled like cabbage. That also could be partially why like water when I would drink it would smell like rubbing alcohol. It was weird, there’s no solution that I came up with it, but it’s another strange thing to look forward to.
Of all of the side effects that I experienced during chemotherapy, the only ones that I still am experiencing 3 years later are weakness in my hands and fatigue. The fatigue partially could be from the anxiety medication that I’m currently on which causes fatigue as one of the side effects, but I was experiencing this fatigue even before I started those anxiety medications. It’s definitely not as bad as when I was on chemo, but I need 8 hours of sleep every night otherwise I am exhausted the next day and need a nap to make it through. I also get tired a lot more easily after exercising, doing housework, or doing yard work.
Do you have any tips or tricks on surviving through the side-effects of chemotherapy? If so help fellow cancer survivors out and let us know in the comments below.
Please make sure that you’ve clicked on the like button right down here so that YouTube knows you’re enjoying my videos and they’ll show them to more people. Also, make sure you’re subscribed so you never miss any of my latest videos and I hope you all are staying safe and healthy, and thanks for watching.
*This video was originally published on June 5, 2020











 friends and in that I got this cute little
friends and in that I got this cute little 


 afternoon the nurse from the oncologist’s office called me to give me instructions on how to take them. She said don’t crush them up and to try as hard as I could to take the dosage 12 hours apart, once in the morning and once in the evening. She also made sure that I knew that I was only supposed to be taking those pills on the days I went in for radiation, so Monday through Friday. I took two pills in the morning and then three pills in the evening 12 hours later. I’m not sure how well you can tell the size of them from this picture but here’s a picture of them next to a juice glass from my last week of chemo.
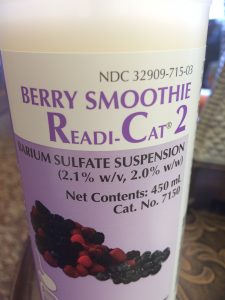
afternoon the nurse from the oncologist’s office called me to give me instructions on how to take them. She said don’t crush them up and to try as hard as I could to take the dosage 12 hours apart, once in the morning and once in the evening. She also made sure that I knew that I was only supposed to be taking those pills on the days I went in for radiation, so Monday through Friday. I took two pills in the morning and then three pills in the evening 12 hours later. I’m not sure how well you can tell the size of them from this picture but here’s a picture of them next to a juice glass from my last week of chemo. June 13th was my first day of radiation and oral chemotherapy and I also had my MRI scheduled for that day. I woke up at 5:45 a.m. to eat a muffin and take the first dose of chemotherapy pills to give me six hours between then and when I was scheduled to be at the hospital for my MRI. I was supposed to check-in at 12:15pm for that MRI at the hospital so if I woke up at 5:45 ate breakfast and the chemo pills I’d be done by 6:15 for sure and that would give me the six hours I needed to fast before the MRI. I tried to go back to sleep but I couldn’t fall asleep I started dozing off once everyone else started waking up so I just got up.
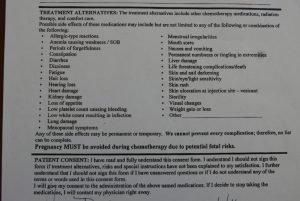
June 13th was my first day of radiation and oral chemotherapy and I also had my MRI scheduled for that day. I woke up at 5:45 a.m. to eat a muffin and take the first dose of chemotherapy pills to give me six hours between then and when I was scheduled to be at the hospital for my MRI. I was supposed to check-in at 12:15pm for that MRI at the hospital so if I woke up at 5:45 ate breakfast and the chemo pills I’d be done by 6:15 for sure and that would give me the six hours I needed to fast before the MRI. I tried to go back to sleep but I couldn’t fall asleep I started dozing off once everyone else started waking up so I just got up. halfway through my treatment. She made it sound like nobody had ever asked that before which I find suspicious, but she said as long as it was in moderation I was okay. Then she went over a list of all the possible side effects of chemotherapy and she even gave me a nice handout that broke it all down based on how common all of the side effects were. She said that the main side effects that most people experience while on Xeloda at varying degrees of severity are more than 25% of patients experience the side-effect of Hand-Foot Syndrome which includes redness and swelling of the hands and feet which can prevent normal activity, cracking and peeling of skin on the hands and feet, and then tingling and numbness or burning again in the hands and feet. Diarrhea was also a common side effect which includes cramping, gas, and bloating which I experienced the diarrhea and the cramping but I’m not sure if it was from the radiation or from the chemotherapy or both of them since I was taking them at the same time.
halfway through my treatment. She made it sound like nobody had ever asked that before which I find suspicious, but she said as long as it was in moderation I was okay. Then she went over a list of all the possible side effects of chemotherapy and she even gave me a nice handout that broke it all down based on how common all of the side effects were. She said that the main side effects that most people experience while on Xeloda at varying degrees of severity are more than 25% of patients experience the side-effect of Hand-Foot Syndrome which includes redness and swelling of the hands and feet which can prevent normal activity, cracking and peeling of skin on the hands and feet, and then tingling and numbness or burning again in the hands and feet. Diarrhea was also a common side effect which includes cramping, gas, and bloating which I experienced the diarrhea and the cramping but I’m not sure if it was from the radiation or from the chemotherapy or both of them since I was taking them at the same time. By the final week of taking the pills the only side effect that I was feeling that I could definitely attribute to the Xeloda was the Hand-Foot Syndrome. It wasn’t as severe as others have gotten it but my hands and feet were red and it was really painful to walk or even stand on my feet. My appetite was pretty low by that last week too. I discovered that if I took the Zofran, even though I wasn’t feeling nauseous taking that did help increase my appetite a little bit. But the side effect from that is that it would constipate me.
By the final week of taking the pills the only side effect that I was feeling that I could definitely attribute to the Xeloda was the Hand-Foot Syndrome. It wasn’t as severe as others have gotten it but my hands and feet were red and it was really painful to walk or even stand on my feet. My appetite was pretty low by that last week too. I discovered that if I took the Zofran, even though I wasn’t feeling nauseous taking that did help increase my appetite a little bit. But the side effect from that is that it would constipate me.
 cancer was we learned that it was Stage 3 Rectal Cancer and that the first step in my treatment was going to be 28 days of radiation therapy and oral chemotherapy. I’ll have the links to the
cancer was we learned that it was Stage 3 Rectal Cancer and that the first step in my treatment was going to be 28 days of radiation therapy and oral chemotherapy. I’ll have the links to the  tumor was, where exactly it was located so he knew he was working off of correct information. He said that the EUS or that rectal ultrasound measured the tumor ranging from four and a half centimeters in, to 15 centimeters in. For us Americans that means the tumor was over four inches long which is like the size of an apple! That sounded huge.
tumor was, where exactly it was located so he knew he was working off of correct information. He said that the EUS or that rectal ultrasound measured the tumor ranging from four and a half centimeters in, to 15 centimeters in. For us Americans that means the tumor was over four inches long which is like the size of an apple! That sounded huge. waiting for my radiation treatment every day. I even got my own special card with a barcode on it so I could beep past that first waiting area and go to the second one. And on the back of this I stuck a picture of Maelle so she could be with me for all of my treatments. On the way down to the room, they showed me the nurse’s station where they would be watching me from for my treatments. Obviously they weren’t allowed to be in the room with me, so there were monitors that had a direct feed of video into the radiation room so they could watch and make sure everything was going as planned in there and then it also had the CT scan of me and then just a couple of other monitors up there.
waiting for my radiation treatment every day. I even got my own special card with a barcode on it so I could beep past that first waiting area and go to the second one. And on the back of this I stuck a picture of Maelle so she could be with me for all of my treatments. On the way down to the room, they showed me the nurse’s station where they would be watching me from for my treatments. Obviously they weren’t allowed to be in the room with me, so there were monitors that had a direct feed of video into the radiation room so they could watch and make sure everything was going as planned in there and then it also had the CT scan of me and then just a couple of other monitors up there. staying on and things getting erased so I just went for the permanent tattoo. They did it right there on the table they just came in with a needle of ink stuck the needle in and just injected the ink and it’s about the size of a freckle but visible enough as you can see.
staying on and things getting erased so I just went for the permanent tattoo. They did it right there on the table they just came in with a needle of ink stuck the needle in and just injected the ink and it’s about the size of a freckle but visible enough as you can see. picture of me, then they went back to the waiting room while I hopped up on the table for treatment. As I mentioned earlier, I had to lay face down for treatment and then I had to pull my pants and my underwear down to my knees. The nurses would hang a towel over my butt so it wasn’t hanging out the whole time, but then they’d tape my butt cheeks apart so that the radiation wouldn’t build up even more and cause worse burns in any folds back there.
picture of me, then they went back to the waiting room while I hopped up on the table for treatment. As I mentioned earlier, I had to lay face down for treatment and then I had to pull my pants and my underwear down to my knees. The nurses would hang a towel over my butt so it wasn’t hanging out the whole time, but then they’d tape my butt cheeks apart so that the radiation wouldn’t build up even more and cause worse burns in any folds back there.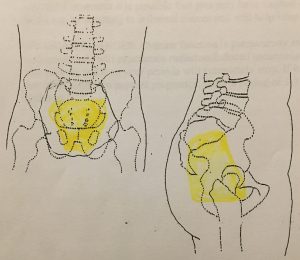 to be treated with radiation. My appointments are scheduled for 15 minutes each day but most of that 15 minutes is spent getting me all perfectly lined up on the table so that they don’t accidentally zap the wrong parts of me during radiation.
to be treated with radiation. My appointments are scheduled for 15 minutes each day but most of that 15 minutes is spent getting me all perfectly lined up on the table so that they don’t accidentally zap the wrong parts of me during radiation. getting so bad it was waking me up in the middle of the night. I was also having bad cramping episodes that would just kind of lay me out on the couch for hours at a time. Week 2 was also when my appetite started to decrease. By the end of the week I had almost a constant feeling of needing to go to the bathroom all the time, but when I would go and try to push something out just blood would come out into the toilet. My pain would rotate through cramps, gas, feeling like I needed to go to the bathroom all the time, and just like my rectum felt sore all the time. The sore rectum was pretty much a constant but those others kind of rotated sometimes would last just for a few minutes other times up to an hour. They would happen often enough that I didn’t feel comfortable going out for a hike or being away from a bathroom for very long.
getting so bad it was waking me up in the middle of the night. I was also having bad cramping episodes that would just kind of lay me out on the couch for hours at a time. Week 2 was also when my appetite started to decrease. By the end of the week I had almost a constant feeling of needing to go to the bathroom all the time, but when I would go and try to push something out just blood would come out into the toilet. My pain would rotate through cramps, gas, feeling like I needed to go to the bathroom all the time, and just like my rectum felt sore all the time. The sore rectum was pretty much a constant but those others kind of rotated sometimes would last just for a few minutes other times up to an hour. They would happen often enough that I didn’t feel comfortable going out for a hike or being away from a bathroom for very long. slower and with the gas pains that were plaguing me and the blood that was passing with the gas, it made it really difficult to run. On my last radiation day, I got this cool certificate and I also got to ring the bell to signify that I was finished with radiation.
slower and with the gas pains that were plaguing me and the blood that was passing with the gas, it made it really difficult to run. On my last radiation day, I got this cool certificate and I also got to ring the bell to signify that I was finished with radiation.