
What is an Ostomy? | Explaining an Ileostomy, Colostomy, and Urostomy
I’ve been talking a lot about ostomies, more specifically my own ileostomy lately, but what in the world are they? Well, it’s time for that video where I explain to you what those ostomies are. If you don’t remember me talking about that you must be new here so welcome to Life as a Cancer Survivor. My name is Jelena and in May of 2016, I was diagnosed with Stage 3 Rectal Cancer. This channel, I created, to give people insight as to what life is like once you hear those words, “you have cancer.” Make sure that if you aren’t subscribed to click the subscribe button right below the video here or in the description below I’ve got the link as well so that you’ll never miss any of my latest videos.
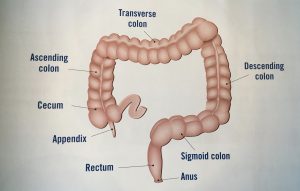 First up let me show you what a picture of the digestive system looks like so here’s this I’ll come back to it here in a moment but this graphic it is from this latest brochure, “Your Screening Guide to Colorectal Cancer” put out by the organization Fight Colorectal Cancer. So let me get back to this graphic so here’s a close up once again this part here this is your large intestine also known as your colon. At the end of the colon that part is called the rectum. At the other end your appendix sticks down there and this squiggly part is your small intestine there’s a lot more of it this is just the last little bit of it this last section of the small intestine it is called the ileum and remember that because I will talk about the ileum again here just in a moment.
First up let me show you what a picture of the digestive system looks like so here’s this I’ll come back to it here in a moment but this graphic it is from this latest brochure, “Your Screening Guide to Colorectal Cancer” put out by the organization Fight Colorectal Cancer. So let me get back to this graphic so here’s a close up once again this part here this is your large intestine also known as your colon. At the end of the colon that part is called the rectum. At the other end your appendix sticks down there and this squiggly part is your small intestine there’s a lot more of it this is just the last little bit of it this last section of the small intestine it is called the ileum and remember that because I will talk about the ileum again here just in a moment.
Now time to talk about ileostomies. This is the kind of ostomy that I had and it’s the most common type that rectal cancer patients receive if they have surgery as part of their treatment plan. It is named an ileostomy after the ileum which is that last section of the small intestine that I just mentioned that connects to your large intestine or to your colon.  There are two different types of ileostomies a loop and a terminal. I had a loop ileostomy which I will use my hand and this hose to demonstrate. My hand will be my abdomen to this is your small intestine. So they cut a slit in your abdomen wall and they pull up a section of your small intestine and cut a slit in it so you see there’s a slit there and they peel that back a little bit or roll it back so it’s actually the inside of your small intestine that you see sticking out. And they sew it into place and this part sticking out is called your stoma.
There are two different types of ileostomies a loop and a terminal. I had a loop ileostomy which I will use my hand and this hose to demonstrate. My hand will be my abdomen to this is your small intestine. So they cut a slit in your abdomen wall and they pull up a section of your small intestine and cut a slit in it so you see there’s a slit there and they peel that back a little bit or roll it back so it’s actually the inside of your small intestine that you see sticking out. And they sew it into place and this part sticking out is called your stoma.
It’s still connected to the rest of your digestive system so a little bit of waste can still come out you still produce mucus and your large intestine that you will occasionally pass but it’s not a daily occurrence. There are no nerve endings in the stoma so it doesn’t hurt when you touch it but there also are no nerve endings there so you can’t control your bowel movements at all it’s just whenever the food is passing through it comes out.

So you’ve seen what it looks like this crude model of what one looks like but let me show you a few pictures of what mine looked like. I warn you this first one may be a little gross because it shows the stoma it’s got stitches and staples so I will let you know when that picture is gone or if you don’t want to watch any of them I’ll let you know when we’re moving on to the next thing so just close your eyes but listen. So here’s the picture the first time that I saw my stoma in the hospital for my first bag change. You can see the little stitches around where the intestine attaches to my abdomen wall and then they had to make the huge incision to take everything out and stapled it shut.
This next picture is a couple of weeks later after I got the staples out my stomach is not swollen from the surgery but you can still see some of the stitches around the stoma and it’s kind of shrank down a little bit, but still um still a decent size.

Since everything is coming out your stoma there that includes gas so that’s stoma does fart and you eat something that gives you a lot of gas at night you might wake up with a balloon sticking off of your tummy like this.
 This is what my stoma looked like with the barrier on it which I will show you a better picture of what the barriers looked like in a moment but this is how mine looked with a barrier. As a souvenir, I saved one set of bags or the bag and barrier. So the barrier is the part that sticks on to you I used a two-piece system so there’s the barrier and the bag. So this is what stuck to me.
This is what my stoma looked like with the barrier on it which I will show you a better picture of what the barriers looked like in a moment but this is how mine looked with a barrier. As a souvenir, I saved one set of bags or the bag and barrier. So the barrier is the part that sticks on to you I used a two-piece system so there’s the barrier and the bag. So this is what stuck to me.
I used the Coloplast brand and I would have to cut the exact size of my stoma on the back here using some special scissors that I got and then this would stick to me. Of course, it’s down on the abdomen not up here on my chest but I also used a convex barrier which I’m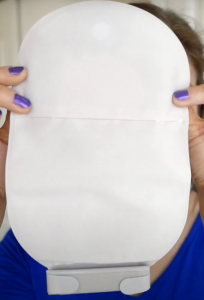 not sure if you can see it very well here but it sticks out a little, it pushes down on your stomach to make the stoma push out a little bit more to make sure none of the waste leaks. So with this one, it actually, here’s the bag and here’s what the bag looks like. So this bag you just peel a sticker off and stick it onto here and there’s your system this folds up and you’ve got the velcro to fold it up so this is what my system looked like on me.
not sure if you can see it very well here but it sticks out a little, it pushes down on your stomach to make the stoma push out a little bit more to make sure none of the waste leaks. So with this one, it actually, here’s the bag and here’s what the bag looks like. So this bag you just peel a sticker off and stick it onto here and there’s your system this folds up and you’ve got the velcro to fold it up so this is what my system looked like on me.
The only difference between the terminal and the loop ileostomy the loop they’ve got the slit cut like I had mentioned the terminal ileostomy, they cut it completely so you’ve got two halves. So there’s just the one end sticking out of your abdomen and then they roll the sides down and sew it in the same way as the other one. So you still have this other bit of your small intestine hanging out in there they’ll sew it to your abdomen wall just so it doesn’t like drift away or anything. This kind can still be reversed but it’s a little more difficult so typically if doctors know that they want to be able to reverse the ileostomy at some point in the future they’ll give you a loop one instead of the terminal one.
Since I personally didn’t have a colostomy, I asked my Instagram friends if any of them that had a colostomy would be interested in talking about their’s with me. Shiray volunteered right away and was more than willing to get on Skype and talk with me and share with you all about what her colostomy is like. She even volunteered to have her mother record a bag change so that we could witness that as well. She was diagnosed at the age of 28 with Stage 3 Rectal Cancer in August of 2016 and after treatment, she was considered NED or having no evidence of disease. However, this past January in 2019 a scan indicated that the cancer had returned and she was considered stage four. After an exhausting year of surgeries and treatment, she currently has no evidence of disease again, yay!! This is my interview with Shiray, and she has a colostomy right now.
 (Jelena) So can you start out by giving us a little background info just about your cancer story?
(Jelena) So can you start out by giving us a little background info just about your cancer story?
(Shiray) Sure, um, so I was originally diagnosed in August of 2016 with stage 3 Rectal Cancer. Um, last year we found out that I was actually restaged to Stage 4 I had some lung mets and liver mets, and so we’ve been spending the last year dealing with that. I got my colostomy bag in between the two stages/chapters.
(Jelena) So then you initially got a loop colostomy right?
(Shiray) I did.
(Jelena) So can you explain to those of us that are unsure about what exactly that is what exactly it is and why that was the right choice for you at the time?
(Shiray) Yeah, so I had kind of an interesting situation. When I first met with my surgeon he told me that I had two options, I had a loop colostomy that I could do or an end colostomy. So my GI and my surgeon were both on the same page that they wanted to try the loop first because it will be easier to reconnect in the future.
(Jelena) Okay.
(Shiray) They were looking forward they really thought that I would only have the bag for like six months, like just enough time to heal, and then I could be reconnected. Well, what ended up happening is during my surgery it started out laparoscopically, and he set me up with a loop colostomy. And so what that is is that they take your colon and they make a slice through it and they bring both ends of that slice up to the surface. And so you end up having like a figure eight or like two holes.
(Jelena) Okay.
(Shiray) And so one end of the intestine comes from your small intestine up to the stoma and then from the stoma down to your rectum is the second portion of it. So what that would mean is that most of my stool would come out of the stoma and go into the bag but since I had that other opening there was a chance that stool could go through that other opening and I would still have regular bowel movements. I was nervous about that because of the pain that I had, but they both agreed so I thought we’ll try it.
And so, during the surgery, while he was finishing up, he was actually leaving the room and the nurse said you need to come back. The loop colostomy kept like falling in through the skin so it wouldn’t stay up on top like it’s supposed to. So he made the decision at that point to open me up and change it to an end colostomy.
(Jelena) Okay.
(Shiray) I never actually lived with the loop but just for a little while. And then an end colostomy is just from your small intestine up to the stoma it’s just one hole the other
section I still have in my body it’s stitched to my abdominal wall. So they can still reconnect me but this is normally used for people who have a permanent colostomy because that other section is pulled out and removed so I still have it in in me.
(Jelena) Okay so that’s what the end colostomy is and that’s what you ultimately ended up with after your surgery.
(Shiray) Yes. People think I’m crazy when I say this, but this is the most convenient thing in the world. I don’t have to run the bathrooms, I don’t have to constantly know where a bathroom is located, I just do what I need to do and we move on.
(Jelena) Yeah. Can you show us what kind of appliances do you use to contain your waste?
(Shiray) Yes, I use a two-piece system from Hollister. It’s a drainable pouch. Okay, so I use this it’s called a flange and you can see it’s got a little bit of a convex there and so what it does is it pushes my stoma out a little further so that the stool actually comes out where it’s supposed to. And then I connect my pouch to it with this little like grommet type thing. They go together and then this is a drainable pouch too so I don’t have to change the whole system I can either take just the bag off and throw it away and put a new one on, I can drain it, or I can change everything.
(Jelena) Okay, so how often do you typically drain it, change the bag, change the whole thing?
(Shiray) So on a normal day, I drain it probably three times. For the most part, I have pretty um oh what’s the word my chemo brain just kicked in,
(Jelena) Like predictable?
(Shiray) Predictable! Thank you. I have pretty predictable output. Typically I will have
a bowel movement like sometime around like 30 minutes after I eat. So I know like I’ve
got usually about an hour afterward I can go and change it and then move on with my day so typically about three times a day.
(Jelena) Okay so you empty it three times a day how often do you change the bag part?
(Shiray) So the bag itself I change it about midweek so I can keep the flange on for a week. It stays on pretty well unless I’ve got like a lot of liquid output that would break down this section I keep it on for a while. The bag though I don’t like the smell after two to three days I changed the bag every two to three days.
(Jelena) Okay, and the bag just clips right off right?
(Shiray) It just pops right off and they come together with this little like grommet and so you can just pull it with one of these tabs. And it just disconnects and I can pop a new one on.
(Jelena) All right. So you mentioned it’s usually like a half-hour after you eat is usually when the output starts and then is it like with a regular human that goes to the bathroom on the toilet like it just comes and then you’re done and it’s quiet for hours until you eat again?
(Shiray) I wouldn’t say that it’s quiet at all. But it is normal in like the output is the same texture as like, a normal bowel movement would be. So since it’s a colostomy I believe ileostomies are more liquid,
(Jelena) Yes,
(Shiray) A colostomy, is just a normal stool that comes out and so it really depends on what I eat and some stuff that you’d have to worry about when you don’t have a colostomy bag. It is really loud though and so that’s the thing that I think I underestimated. I think that I believed that I could control that at some point you know you can hold in farts and gas you can’t do that with a colostomy it comes out when it wants to it makes whatever noise it wants to and you just have to get used to it.
(Jelena) Yes. So you have no feeling when it’s coming out right?
(Shiray) None.
(Jelena) So you have no idea and you can’t like hold it.
 (Shiray) No, and the only time I can feel something is if this lifts off of my skin. I can feel it then because I can feel it being pushed out so I know it’s something like I know I’m about to have a leak or something’s happening but most of the time I have no clue it’s coming.
(Shiray) No, and the only time I can feel something is if this lifts off of my skin. I can feel it then because I can feel it being pushed out so I know it’s something like I know I’m about to have a leak or something’s happening but most of the time I have no clue it’s coming.
(Jelena) Okay. Are there other things that you want to mention about it?
(Shiray) Yes! I was really worried. I know initially, I said I didn’t want to have a bag like when I woke up from surgery I was like “yay!” I realized that I can do so much more with a bag than I was able to do before I had the bag because I ended up, um you know before like I said I was homebound, I couldn’t leave my house, if I did leave I had to know where a bathroom was or have a change of clothes. With the bag I’ve been able to lift weights, I can swim, I can still be a normal functioning 28-year-old human, 29-year-old human.
It’s, I think it’s important that people understand that this doesn’t limit you in any way. You can limit yourself and you have to be more cautious about it. Like when I was lifting I had to work with a trainer who taught me the right form and she really made sure that my core was strong so that when I did do those heavy lifts it’s not like I was putting myself in danger. You just have to be smart about it but you can do anything with it.
(Jelena) Uh-huh. Uh, so let’s see, so how long have you had the colostomy now?
(Shiray) So I’ve had it a little over three years.
(Jelena) Okay, so you’ve had it for quite a while.
(Shiray) I have.
Shiray had so many great things to share with me that I couldn’t fit it all in this video, so stay tuned next week to hear even more from her and to see how she changes her colostomy bag.
Then last but not least is a urostomy which allows urine to exit the body through a stoma.
This one is the least common of the three ostomies that colorectal cancer patients receive and actually I didn’t know how the stoma was even formed until I did some research for this video. There are multiple techniques used to create a urostomy but I’ll just talk about the most common one which is the one that has the highest patient satisfaction rate and the lowest complication rate and that one is called the ileal conduit.
So for this type of urostomy they actually use the small intestine. So back to my tube here let’s say it’s all connected so what they do is they cut off that ileum part so the end of the small intestine is completely separated from the rest and they sew one end shut and the other end sticks out of your abdomen wall to create the stoma, it’s folded over, sewn to the abdomen wall just like the ileostomy. On that sewn up end, say that these are your ureters which are those tubes that will go from your kidneys down to your bladder so they disconnect them from the bladder and they insert them in at the end here. This is sewn up so the urine will pass through the small intestine and out the stoma.
A bag is worn for this type of ostomy also, but the bag itself is a little bit different it’s got more of like a tube drain at the end rather than a larger opening like on the colostomy and ileostomy bags just because if you have an opening that’s this large dumping urine out is just gonna splash all over the place so they’ve got more of a drainage system for the urostomy bags.
So those are the three types of ostomies that a colorectal cancer patient may get after their diagnosis. I hope that cleared up a little bit what each of the different ostomies are. Let me know in the comments below something that you learned from this video about the ostomies. I learned that the stoma for urostomy is made from the small intestine. I always assumed that it was made out of some part of your original urinary system.
If you happen to have missed my diagnosis video and are unsure why I need an ileostomy, there’s the link click on that or the link will also be in the description below so that you can get caught up to speed on that. If you learned something new in this video I’d love it if you hit the like button for me, and thanks for watching I’ll see you next week.
2 thoughts on “What is an Ostomy?”