
What is FOLFOX Chemotherapy?
Welcome back to Life as a Cancer Survivor. In this video, I’ll talk about the basics of the IV chemotherapy FOLFOX, which is commonly given for Stage 3 Rectal Cancer patients. I’ll talk about what the drugs are that are in it, how they’re administered, and the side effects that I experienced. In another video, I’ll dive even deeper into those side effects and also give you hints on how I coped with a lot of those side effects. My name is Jelena and I was diagnosed with Stage 3 Rectal Cancer in May of 2016.
So a week and a half before I was scheduled to begin chemotherapy I had another chemo training class which was just an appointment with my Oncologist’s Physician Assistant. So at that appointment, I got this folder of information which included my current medication list, a packet of information on FOLFOX, and a separate handout just on oxaliplatin and neuropathy. So the first of those sheets that I’ll go over is my current medication list.
The only thing that I was taking at the time was vitamin D for a deficiency that I had before I was diagnosed with cancer. But in addition to that, they added three more medications to that list. The first one was Zofran, an anti-nausea medication, and that one I was supposed 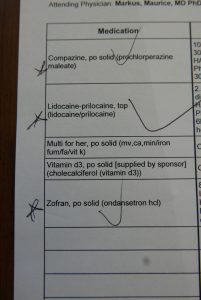 to take just a few hours after I got home from my chemotherapy infusions that evening to help keep the nausea at bay and under control. And I was supposed to take that for 2 to 3 days following the infusion. The second prescription was for Compazine and that one is also an anti-nausea medication and that one I was supposed to use for breakthrough nausea so if in between the doses of Zofran it wasn’t enough I was supposed to take Compazine as an additional tool in my box to try and keep the nausea under control. Then the third prescription was for lidocaine which is a numbing cream. I spoke about this one in my port video, I was supposed to put the cream over the port site before a needle was inserted into it for blood draws or for chemotherapy so that it was numb and I wouldn’t feel it at all.
to take just a few hours after I got home from my chemotherapy infusions that evening to help keep the nausea at bay and under control. And I was supposed to take that for 2 to 3 days following the infusion. The second prescription was for Compazine and that one is also an anti-nausea medication and that one I was supposed to use for breakthrough nausea so if in between the doses of Zofran it wasn’t enough I was supposed to take Compazine as an additional tool in my box to try and keep the nausea under control. Then the third prescription was for lidocaine which is a numbing cream. I spoke about this one in my port video, I was supposed to put the cream over the port site before a needle was inserted into it for blood draws or for chemotherapy so that it was numb and I wouldn’t feel it at all.
The next packet of information I received was all about FOLFOX, the IV chemotherapy I was going to be receiving. FOLFOX is actually 3 different drugs mixed together. It is 5-fluorouracil, also known as 5-FU, oxaliplatin, and leucovorin. The 5-FU and oxaliplatin are chemotherapy drugs that prevent the division and growth of cancer cells and causes them to shrink and die. The leucovorin helps increase the efficiency or the efficacy of the 5-FU. When I would go in for chemotherapy infusions, all three drugs would be given to me over the span of about 3 hours plus anti-nausea medications at the very beginning. The way it was divided up, at the very beginning for the first 15 to 20 minutes would just be an infusion of anti-nausea meds, then for the next two to two and a half hours it was the chemotherapy drugs, then they would disconnect me from that and they would connect a portable pump to me through the port and I would take that pump home and over the next two days I would continue to receive an infusion of 5-FU. Then after those 2 days I would return to the cancer center and they would disconnect me from the pump. That’s what I had to look forward to every two weeks for 8 cycles.
going to be receiving. FOLFOX is actually 3 different drugs mixed together. It is 5-fluorouracil, also known as 5-FU, oxaliplatin, and leucovorin. The 5-FU and oxaliplatin are chemotherapy drugs that prevent the division and growth of cancer cells and causes them to shrink and die. The leucovorin helps increase the efficiency or the efficacy of the 5-FU. When I would go in for chemotherapy infusions, all three drugs would be given to me over the span of about 3 hours plus anti-nausea medications at the very beginning. The way it was divided up, at the very beginning for the first 15 to 20 minutes would just be an infusion of anti-nausea meds, then for the next two to two and a half hours it was the chemotherapy drugs, then they would disconnect me from that and they would connect a portable pump to me through the port and I would take that pump home and over the next two days I would continue to receive an infusion of 5-FU. Then after those 2 days I would return to the cancer center and they would disconnect me from the pump. That’s what I had to look forward to every two weeks for 8 cycles.
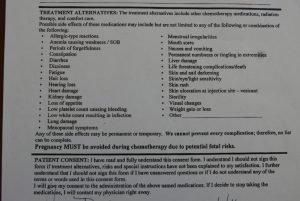 On the consent form that I had to sign, let me show you it has a long list of just general chemotherapy side-effects that no matter what chemo you’re on you could experience. And those are just for general chemo. In addition to that, there’s also information in the FOLFOX packet it had even more side effects that were specific to FOLFOX. Now here’s the highlighted list of all of the side effects from that consent form that I experienced: diarrhea, fatigue, hair loss. I didn’t lose all of my hair but it thinned quite a bit, loss of appetite, low platelet count, low white count, menstrual irregularities, nausea, numbness and tingling in extremities, and weight loss. From the FOLFOX packet, it listed even more side effects and it separated them out based on whether they were common which means 25% or more of patients experienced it, down two rare which means less than 5% experienced it. From that list, I experienced: throat pain, difficulty swallowing or eating, muscle cramps, metallic or medicinal taste, and trouble sleeping.
On the consent form that I had to sign, let me show you it has a long list of just general chemotherapy side-effects that no matter what chemo you’re on you could experience. And those are just for general chemo. In addition to that, there’s also information in the FOLFOX packet it had even more side effects that were specific to FOLFOX. Now here’s the highlighted list of all of the side effects from that consent form that I experienced: diarrhea, fatigue, hair loss. I didn’t lose all of my hair but it thinned quite a bit, loss of appetite, low platelet count, low white count, menstrual irregularities, nausea, numbness and tingling in extremities, and weight loss. From the FOLFOX packet, it listed even more side effects and it separated them out based on whether they were common which means 25% or more of patients experienced it, down two rare which means less than 5% experienced it. From that list, I experienced: throat pain, difficulty swallowing or eating, muscle cramps, metallic or medicinal taste, and trouble sleeping.
Then I also got these two handouts on oxaliplatin and neuropathy. The oxaliplatin can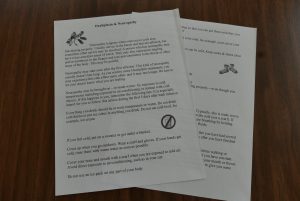 cause nerve damage in the extremities, so your hands and your feet, and that nerve damage is what can cause neuropathy. In case you’re unfamiliar with what neuropathy is, it’s defined as a tingling, weakness, burning, and pain in the hands and the feet. A common cause is diabetes, but many chemotherapies including oxaliplatin can cause neuropathy as well. It can start as soon as during your chemotherapy infusion, but typically it will go away after a few days. I got tingling in both my hands and in my feet but the hands they would get better within a few hours after the infusion. The feet however, that tingling turned into some burning and pain which lasted two years after I finished my last infusion. The neuropathy is definitely something that you want to keep your doctor posted on. Think of it kind of like radiation burns. The worse they get, the harder it is to recover from, and they don’t go away after you finish treatment. Other weird neuropathy side effects that you can experience with the oxaliplatin is just a general extreme cold sensitivity. As you can see in this picture, I had a water bottle with me at my very first
cause nerve damage in the extremities, so your hands and your feet, and that nerve damage is what can cause neuropathy. In case you’re unfamiliar with what neuropathy is, it’s defined as a tingling, weakness, burning, and pain in the hands and the feet. A common cause is diabetes, but many chemotherapies including oxaliplatin can cause neuropathy as well. It can start as soon as during your chemotherapy infusion, but typically it will go away after a few days. I got tingling in both my hands and in my feet but the hands they would get better within a few hours after the infusion. The feet however, that tingling turned into some burning and pain which lasted two years after I finished my last infusion. The neuropathy is definitely something that you want to keep your doctor posted on. Think of it kind of like radiation burns. The worse they get, the harder it is to recover from, and they don’t go away after you finish treatment. Other weird neuropathy side effects that you can experience with the oxaliplatin is just a general extreme cold sensitivity. As you can see in this picture, I had a water bottle with me at my very first infusion and I always brought one with me because I would be there for a few hours. Within about a half-hour of starting the chemo part of the infusion the first side effect kicked in. When I took a sip from my water bottle when I swallowed it felt like I was swallowing glass. It startled me because I wasn’t quite sure what to expect with that cold sensitivity. From that point, until about 5 days after my infusion, it was no cool and not even room temperature drinks, it all had to be warm otherwise it feel like the glass going through my throat when I would swallow.
infusion and I always brought one with me because I would be there for a few hours. Within about a half-hour of starting the chemo part of the infusion the first side effect kicked in. When I took a sip from my water bottle when I swallowed it felt like I was swallowing glass. It startled me because I wasn’t quite sure what to expect with that cold sensitivity. From that point, until about 5 days after my infusion, it was no cool and not even room temperature drinks, it all had to be warm otherwise it feel like the glass going through my throat when I would swallow.
The handouts also gave multiple other tips or hints on how to deal with the cold sensitivity. So it notes in there make sure that everything that you eat or drink is at room temperature or warm, if you feel cold put on a sweater or get under a blanket, duh, I think that’s obvious for anybody that’s not even on chemotherapy. Cover up when you’re outdoors, always wear a scarf over your nose and your mouth, avoid direct exposure to air conditioning, which, um, I could avoid air conditioning but the extreme cold was hard to avoid because I was getting treatment in winter in Colorado, don’t use an ice pack on any part of your body, keep a pair of gloves in the kitchen for handling things in the refrigerator, and then also keep socks or slippers nearby all the time for walking on tile and linoleum, wood floors also.
There’s also a thing that many people call “first bite syndrome,” which you’ll most likely experience after each infusion. It always happened to me and it was always the first bite that I took of something after I left the cancer center. It was like a really stiffness and pain in the jaw but it only happened for that very first bite. It made a kind of difficult to chew the first bite but then after you swallowed it and took another bite everything was fine so it was really strange and weird but that’s something to also watch out for.
For me, the oxaliplatin is what caused the worst of the side effects. How do I know this? Well, for my final treatment number eight they left the oxaliplatin out completely because the tingling in my feet was getting worse so instead of damaging the nerves even more they left it out. After that infusion I didn’t have any of the extreme cold sensitivity side effects like I had had after other infusions.
The schedule of appointments went like this around each infusion. A day or two before I would go in to get my blood drawn. I would go down to the cancer center for this because I wanted the nurses down there to access my port for it because I could numb the port and I wouldn’t feel it, but also within a half-hour to an hour after the blood draw appointment (because they do it by appointment at the cancer center) I would have an appointment with my Oncologist’s Physician Assistant to go over those results. So it was just easier to have it all done right there and at that appointment with the PA she would go over the blood test results, basically just summarizing the things that they were looking at to make sure that my body was healthy enough to receive chemo the next day. So the platelets were the one thing that dropped a lot for me, so that was the one thing they would keep an eye on. The platelets are what’s in your blood that cause it to clot, so when your platelets get really low even a small cut could turn into an emergency because the blood won’t clot and it won’t stop bleeding.
Then the following day I would come back for chemo. I went back and got to choose whatever chair I wanted in there so I would always go over into the corner by the window so that I could look out at the mountains. I got settled in for 3 hours or so and then got the pump attached to me to take home. Here’s a picture of what it looked like and it came with its own set of instructions just in case you needed to know how to work it. All I needed to know how to do was how to shut it off when it started beeping when the chemo was done. Then I was also sent home with this Hazmat kit. It was very comforting to know that what they were injecting into me needed cleaned up with a Hazmat kit. Then they also gave me both an over-the-shoulder bag or a fanny pack that I could choose from to where the pump in. I chose the over-the-shoulder
whatever chair I wanted in there so I would always go over into the corner by the window so that I could look out at the mountains. I got settled in for 3 hours or so and then got the pump attached to me to take home. Here’s a picture of what it looked like and it came with its own set of instructions just in case you needed to know how to work it. All I needed to know how to do was how to shut it off when it started beeping when the chemo was done. Then I was also sent home with this Hazmat kit. It was very comforting to know that what they were injecting into me needed cleaned up with a Hazmat kit. Then they also gave me both an over-the-shoulder bag or a fanny pack that I could choose from to where the pump in. I chose the over-the-shoulder  bag because the fanny pack was way too big around my waist and it was a fanny pack. So I wore that pump for 2 days. My chemotherapy was always on Tuesdays so I would go in at the end of the day on Thursdays, I would have to go back to the cancer center to get the pump disconnected from me. This was my schedule every other week for 8 cycles.
bag because the fanny pack was way too big around my waist and it was a fanny pack. So I wore that pump for 2 days. My chemotherapy was always on Tuesdays so I would go in at the end of the day on Thursdays, I would have to go back to the cancer center to get the pump disconnected from me. This was my schedule every other week for 8 cycles.
I hope you learned a little bit more about what FOLFOX is and the basics of IV chemotherapy. I’m going to do a future video on more specifics of the side effects that I experienced and how I coped with them so make sure that you’re subscribed so you don’t miss that video. In my previous video, I talked about what it was like to get a port placed, so if you missed that one you can click here and that’ll take your right over to that video. Make sure that you click on the like button though if you enjoyed this video and please share it with anybody that you think also might enjoy it. Thank you guys so much for all your support and thanks for watching.
*This video was originally published on May 22, 2020